Bone & Muscle Problems
© American Institute for Preventive Medicine
Bone & Muscle Problems
© American Institute for Preventive Medicine
Bone & Muscle Problems
Fibromyalgia is a chronic, arthritis-like illness. It affects the muscles, not the joints.
Signs & Symptoms
* Chronic widespread pain on both sides of the body. This lasts for at least 3 months. It is not due to any other problem. Muscle pain can be severe.
* Pain in 11 or more of 22 “tender points.” (These are shown at right.)
* Fatigue. Disturbed sleep. Anxiety. Depression.
These symptoms are also linked to fibromyalgia:
* Memory lapses. Problems concentrating. Feeling confused.
* Chronic headaches. Jaw pain. A tingling feeling in the limbs.
* Irritable bowel. Swelling and pain in the abdomen. Gas. Constipation. Diarrhea.
Causes
The exact cause is not known. Factors thought to play a role include:
* An illness caused by an infection. Emotional or physical trauma.
* Hormones. Women are affected more often than men.
* Brain chemicals and muscles don’t function like they should.
Treatment
* Exercise therapy.
* Medication to treat symptoms.
* Massage therapy.
Questions to Ask
Self-Care / Prevention
* Follow the treatment plan advised by your doctor.
* Use biofeedback.
* Use relaxation techniques. Meditate.
* Take warm baths.
* Use a heating pad.
* Massage sore muscles.
Resources
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Bone & Muscle Problems
Some foot problems are due to years of wear and tear on your feet. Others can be due to shoes that do not fit well or trimming your toenails too close to your skin. Circulation problems and diseases, such as diabetes, can lead to foot problems, too.
{Note: If you have diabetes or circulation problems, contact your doctor for any foot problems.}
To Help Prevent Foot Problems
* Maintain a healthy weight to avoid excess strain on your feet.
* Wear shoes that fit well. Don’t wear shoes with pointed toes or ones that fit too tightly.
* Wash and dry your feet daily.
* Keep your feet moisturized.
* Inspect your feet daily for signs of problems.
* Rest your feet by elevating them.
* Persons with diabetes and/or circulation problems need to take special care of their feet. Good foot care can prevent some foot infections. It may be necessary for a health care professional to cut the toenails.
R.I.C.E.
* Rest the injured area for 24 to 48 hours.
* Ice the area as soon as possible. Keep doing this for 10 minutes every 2 hours for the first 48 hours. Use an ice pack, ice in a heavy plastic bag with a little water, a bag of frozen vegetables, etc. Put a thin towel between the ice pack and the skin.
* Compress the area. Wrap with an elastic bandage. Do not cut off circulation. Remove the bandage every 3 to 4 hours, for 15 to 20 minutes each time.
* Elevate the area above heart level, if possible. Place it on a pillow, folded blanket, stack of newspapers, etc.
Athlete’s Foot
Signs & Symptoms
Moist, soft, red, or gray-white scales on the feet, especially between the toes. Cracked, peeling, dead skin area. Itching. Sometimes small blisters on the feet.
What to Do
SeeAthlete’s Foot.
Blisters

Signs & Symptoms
Red, sometimes fluid-filled sores caused by shoes that rub the foot.
Self-Care / Prevention
* Don’t break a blister. If it breaks on its own, apply an antibacterial spray or ointment and cover with a bandage or sterile dressing.
* Don’t cut away or pull off the broken blister’s loose skin. This protects the new skin below it.
Broken Bone(s) in the foot (not just a toe).

Signs & Symptoms
Pain from a fall or injury to your foot (not just a toe) with any of these problems:
* Severe bleeding.
* Your foot is misshaped.
* You can’t move your foot.
* Your foot looks blue or pale and is cold and numb.
* Your foot is so painful and/or swollen that you can’t put any weight on it.
What to Do
Get medical care fast!
Broken or Sprained Toe

Signs & Symptoms
Pain in only one toe after an injury to the toe.
Buerger’s Disease
Signs & Symptoms
Open sores (ulcers) on the toes. Pain on the instep and cold, pale skin color which improves with rest.
What to Do
See doctor.
Bunion

Signs & Symptoms
The big toe points inward or outward. A bony bulge at side of the big toe. Thickened skin. Possible fluid build-up near the big toe. Stiffness or pain.
Self-Care / Prevention
* Don’t wear high heels or shoes with narrow toes.
* Wear sandals.
* Use moleskin or padding to separate overlapped toes.
* Try arch supports to reduce pressure.
* Use ring-shaped pads over a bunion.
* Cut out an old pair of shoes to wear in the house.
* Soak your feet in warm water.
* If needed, take an over-the-counter pain reliever as directed.
Callus
Signs & Symptoms
Thickened skin on the ball or heel of the foot. Usually no pain.
Cellulitis
Signs & Symptoms
The bottom of the foot is red and swollen and feels warm and tender.
What to Do
SeeCellulitis.
Corn
Signs & Symptoms
Thickened skin on tops of and between toes where rubbing is constant. Feels hard to the touch and looks round. Small, clear spot (hen’s eye) may appear in the center.
Cut or Puncture Wound
Signs & Symptoms
Cut or puncture from a dirty or contaminated object, such as a rusty nail or other object in the soil.
Foot Cramp
Signs & Symptoms
Charley horse or muscle spasm in the foot. Often, this occurs at bedtime.
Self-Care / Prevention
* Stretch the foot muscles.
* Pull the foot back into a flexed position.
* Push the foot into the floor.
Frostbite (if signs occurs after cold exposure).
Signs & Symptoms
Toes turn white then red in response to cold. Tingling. Numbness.
What to Do
Contact doctor for an appointment right away.
Gangrene

Signs & Symptoms
These problems appear in a matter of hours to a few days:
* The skin of your foot or toe is gray to black in color.
* You cannot feel sensation in your foot.
What to Do
Get medical care fast!
Gout
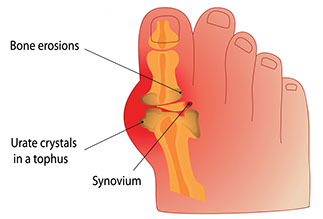
Signs & Symptoms
Severe pain in foot joint, often the big toe. The pain is not due to an injury. The joint hurts a lot when anything touches it. The area is red, swollen, and tender.
What to Do
See doctor.
Hammertoe

Signs & Symptoms
Curled or claw-like position in a toe (usually the 2nd toe). A corn forms on the top of the toe. Pain.
Self-Care / Prevention
* Wear wide, roomy shoes.
* Massage the toes or get a foot rub.
* Change shoes during the day. Try athletic shoes.
* Use small pads over the center of the toe to lessen pressure.
Heel Spur
Signs & Symptoms
Tenderness and pain under the heel bone.
What to Do
See doctor.
Self-Care / Prevention
* Use a cushion or heel cup under the heel.
* Do not jog or run. Avoid prolonged standing.
* Lose weight, if overweight.
* Roll a tennis ball under ball of the foot.
* Put ice on the heel for 10 minutes. Remove it for 10 minutes. Repeat many times.
* If needed, take an over-the-counter pain reliever as directed.
Infection
Signs & Symptoms
A foot wound with: Fever; redness, tenderness, or warmth; swelling; pain; and/or pus.
What to Do
See doctor.
Self-Care / Prevention for Minor Infections
* Soak the foot in warm, soapy water for 20 minutes, 4 to 6 times a day. Pat the infected area dry. Use extra care if you have peripheral vascular disease. Make sure the water is not hot.
* Apply an over-the-counter antibiotic ointment, such as Neosporin. Cover with a sterile cloth or bandage.
Ingrown Toenail
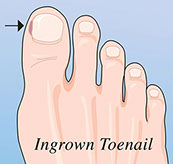
Signs & Symptoms
Discomfort, pain, tenderness, and/or redness under the corner of a toenail and nearby skin.
Morton’s Neuroma
This is thickening of nerve tissue, usually between the third and fourth toes.
Signs & Symptoms
Sharp and burning pain on the ball of the foot.
Self-Care / Prevention
* Wear wide shoes with soft insoles.
* Put pads or arch supports in your shoes. These help take pressure off the area.
* Take an over-the-counter medicine for pain as directed.
* See your doctor if the above measures don’t bring relief.
Peripheral Vascular Disease
Signs & Symptoms
Sudden onset of pain in your feet and legs. The skin on your feet rapidly changes color: white, red, blue, grayish, or black.
What to Do
Get medical care fast!
Planter Fasciitis
This is a problem with ligaments and tissues in the foot arch.
Signs & Symptoms
Pain between the heel and the ball of the foot. Often this is due to walking, running, or putting weight on the foot.
Self-Care / Prevention
* Rest the foot as much as you can.
* Use R.I.C.E.
* Take an over-the-counter medicine for pain and swelling as directed.
* Wear shoes with a solid arch support.
Planter Wart
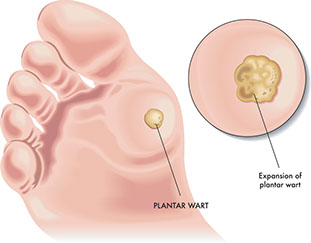
Signs & Symptoms
Painful growth on the ball or heel of the foot. Black pinholes or spots in the center.
Self-Care / Prevention
* Try salicylic acid plasters or other over-the- counter products, such as Wart-Off. Follow package directions.
* Use cushions in shoes.
* Wash your hands after touching warts to avoid re-infection.
* Wear sandals in the shower or public areas, such as pools.
* Do not pick at plantar warts.
Rheumatoid Arthritis
Signs & Symptoms
Joint pain and morning stiffness in joints that lasts more than 1 hour. Fatigue.
What to Do
See doctor.
Toenail Fungus
Signs & Symptoms
White, brown, or yellow toenail. The nail can thicken, then get soft and weak. It may tear away from the nail bed or look deformed.
What to Do
See doctor.
Bone & Muscle Problems
Pain in the legs or ankles can range from mild to severe. The type and amount of pain depends on the cause.
For Pain, in General
* Take an over-the-counter medicine for pain as directed on the label. If the pain is not better after a few doses, call your doctor.
* Use a heating pad (set on low), a hot pack, or a moist, warm towel on the area of pain. If the pain is due to an injury, don’t use heat for 48 hours. Use R.I.C.E.
To Help Prevent Leg Pain & Ankle Pain
* Get to and stay at a healthy weight.
* Get regular exercise. This helps to keep ankle and leg muscles strong.
* Before you exercise, stretch and warm up your muscles. When you are done, cool them down.
* Protect your knees. Use knee pads when you garden or kneel. Always land on bent knees when jumping. Avoid deep knee bend exercises.
* Don’t wear high-heeled shoes. Keep your shoes in proper shape.
* Take good care of your feet.
R.I.C.E.
* Rest the injured area for 24 to 48 hours.
* Ice the area as soon as possible. Keep doing this for 10 minutes every 2 hours for the first 48 hours. Use an ice pack, ice in a heavy plastic bag with a little water, a bag of frozen vegetables, etc. Put a thin towel between the ice pack and the skin.
* Compress the area. Wrap with an elastic bandage. Do not cut off circulation. Remove the bandage every 3 to 4 hours, for 15 to 20 minutes each time.
* Elevate the area above heart level, if possible. Place it on a pillow, folded blanket, stack of newspapers, etc.
Baker’s Cyst
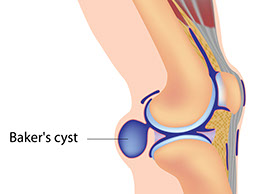
Signs & Symptoms
Painless or painful swelling behind the knee. May feel like a water-filled balloon.
What to Do
Call doctor.
Broken Bone or Dislocation

Signs & Symptoms
Any of the signs that follow occur after a leg or ankle injury. A bone sticks out or bones in the injured limb make a grating sound. The injured limb looks deformed, crooked, or the wrong shape. You lose feeling in the injured limb. The skin under the affected injured area is cold and blue. The limb is very painful and/or swollen or you can’t bear weight on the limb or move it.
Bursitis
Signs & Symptoms
Pain and swelling around a knee or hip joint. The pain gets worse with movement. Fever (maybe).
What to Do
See doctor.
Deep-vein thrombosis (DVT) with or without a blood clot to the lung
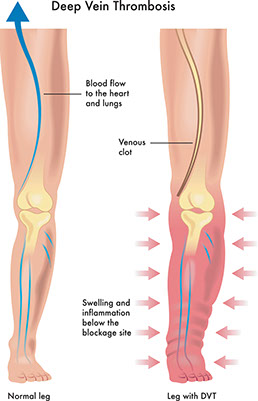
Signs & Symptoms
Pain, redness (may have shades of red, purple, and blue), or swelling in one ankle or leg. May be followed by severe shortness of breath that came on all of a sudden. May include coughing up blood or pink-frothy sputum. Chest pain.
What to Do
Get medical care fast!
Flu
Signs & Symptoms
Aches in leg muscles and joints with fever and/or chills. Headache. Dry cough. Sore throat. Fatigue.
Gout
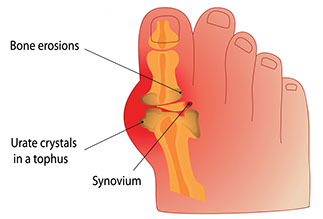
Signs & Symptoms
Sudden, severe pain in a toe, knee, or ankle joint. The pain can be felt even when clothing is rubbed against the joint. The joint area is swollen, red, or purplish in color. It also feels warm, and is very tender to the touch.
What to Do
See doctor.
Heart Failure

Signs & Symptoms
Swelling of both ankles at the same time. Shortness of breath. May have a dry cough or a cough with pink, frothy mucus.
What to Do
Get medical care fast!
Infection. Could also be Cellulitis.
Signs & Symptoms
Pain with fever, redness, tenderness, warmth and pus at a wound site. A red streak up the leg (rarely).
What to Do
See doctor.
Leg Cramp
Signs & Symptoms
Sudden, sharp, tightening pain in the leg, often the calf. The muscle feels hard to the touch. The pain subsides after a minute or so and the muscle relaxes.
Self-Care
* Walk on the leg.
* Shake the leg and then elevate it.
* Sit with your leg flat on the floor. Flex your foot upward, then toward your knee. Reach for your toes and pull them toward your knee. This stretches the calf muscles.
* Have someone massage the cramped muscle gently, but firmly.
* Apply a heating pad (set on low), a hot pack, or moist, warm towel to the muscle cramp.
* Rub the muscle that is cramping. Rub upward from the ankle toward the heart.
(Note: Do not rub a leg if you suspect phlebitis or thrombosis.)
To Prevent Leg Cramps
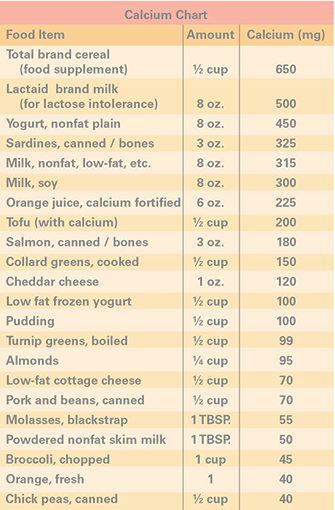
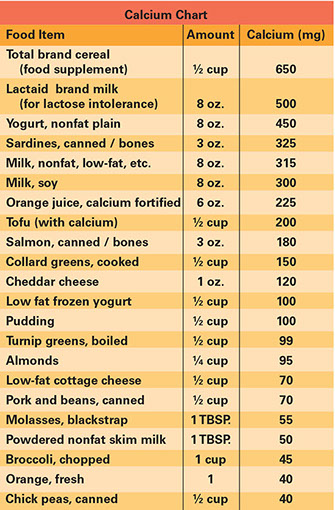
* Get good sources of calcium, potassium, and magnesium. See lists at left. Take calcium, potassium, and magnesium as advised by your doctor.
* Drink plenty of water and other fluids. Limit drinks with caffeine. Avoid drinks with alcohol. Doing these things can help prevent dehydration which could cause leg cramps.
* Warm up your muscles before you exercise. Cool down your muscles when you are done.
* With your doctor’s okay, wear elastic stockings while you are awake.
* Another way to stretch your calf muscles is to ride a stationary bicycle for a few minutes.
* Take a warm bath before bedtime.
* Sleep with loose-fitting blankets and night clothes. Keep your legs warm.
* If you have severe leg cramps or get them often, tell your doctor. Ask if any medication you take could cause your leg cramps. Ask for ways to treat your leg cramps.
* Before you go to bed, stretch your calf muscles. Here’s one way to do this:
– Stand an arm’s length away from a wall. Lean against it with the palms of your hands.
– Bend your left knee. Keep your right leg straight behind you. Keep both feet flat on the floor and your back straight.
– Lean forward. Feel your right calf muscle stretch. Hold the stretch as you count to 10 slowly.
– Repeat, switching leg positions.
Lyme Disease
Signs & Symptoms
Muscle or joint pain and chronic swelling of the knee joints. These problems develop months or years after a deer-tick bite and a bulls-eye red rash with pale centers.
What to Do
See doctor.
Osteoarthritis
Signs & Symptoms
Pain, stiffness, and sometimes swelling of the knee or ankle joints. Often, the joint has gotten tender over months or years and may look enlarged or deformed.
Osteoporosis
Signs & Symptoms
Leg or ankle pain with gradual loss of height; stooped posture; backache; and/or past bone fractures, especially in the wrists and hips.
Paget’s Disease
This is a bone disorder that progresses slowly. Most persons with this disease do not develop symptoms.
Signs & Symptoms
Leg pain that radiates from the lower back. Pain or stiffness in the knees. Bowing of the legs or other bone deformity. Unexplained bone fractures. May have headache, dizziness, hearing loss, and/or ringing in the ears.
What to Do
See doctor.
Self-Care / Prevention
* If needed, take an over-the-counter medicine for pain as directed on the label.
* Take other medicines as prescribed by your doctor.
* Get regular checkups to detect hearing loss.
Peripheral Vascular Disease
Signs & Symptoms
Sudden and severe pain in a leg that is not relieved with rest.
What to Do
Get medical care fast!
Signs & Symptoms
Muscle pain in one or both legs. Fatigue in the thighs, calves, and feet. This improves with rest. Open sores on the lower leg, ankles, or toes. Weak or no pulse in the affected limb. Cold or numb feet. Pale, bluish-colored toes.
What to Do
See doctor.
Sciatica
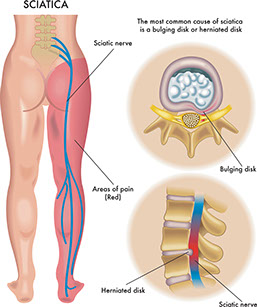
Signs & Symptoms
Sharp pain from the buttocks down the leg. Numbness and tingling in the leg.
Sprain, Strain, or Sport Injury
Signs & Symptoms
Pain in the leg or ankle after an injury that does not keep you from moving the limb.
Rheumatoid Arthritis

Signs & Symptoms
Pain, stiffness, and swelling, usually in both knees or ankle joints. The joint looks deformed. Weakness and fatigue. Dry mouth and dry, painful eyes.
Varicose Veins
Signs & Symptoms
Pain or itching in the legs with swollen and twisted veins that look blue and are close to the surface of the skin. The veins bulge and feel heavy. Swelling in the legs and ankles.
Bone & Muscle Problems

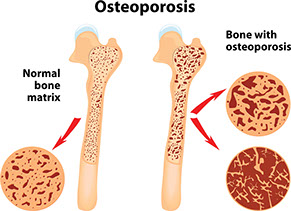
Osteoporosis is a loss of bone mass and strength. This significantly increases the risk of fractures and falls.
To help prevent osteoporosis, take medicines as prescribed by your doctor, do weight-bearing exercises, choose a balanced diet rich in calcium and vitamin D, and practice good posture.
Often, the first sign of osteoporosis is a fracture of a wrist, hip, or spine.
To help detect osteoporosis, have tests that measure bone density as advised by your doctor.
If you have been diagnosed with osteoporosis or had a fracture from a fall at standing height, talk with your doctor about medication options. Also, learn how to fall-proof your home. Learn more about bone health and osteoporosis atnof.org.
Bone & Muscle Problems
Osteoporosis is a loss in bone mass and bone strength. Bones become less dense. This makes them weak and easier to break. Any bone can be affected. The hips, wrists, and spine are the most common sites.
Signs & Symptoms
Osteoporosis is a “silent disease.” It can occur without pain. You don’t see or feel changes taking place inside your bones. Often, the first sign is a fracture of the hip, wrist, or spine. When signs and symptoms occur, they include:
* Gradual loss of height
* Rounding of the shoulders
* Sudden back pain
* Stooped posture
* Dowager’s hump
Causes & Risk Factors
Bone is living tissue. It breaks down and is replaced with new bone. Osteoporosis occurs when new bone does not replace old bone fast enough.
Risk Factors
* Being female. Women are more likely to develop osteoporosis than men.
* Low estrogen level. This occurs with menopause.
* Low testosterone level in men
* Aging
* A family history of osteoporosis or broken bones as adults
* Having a thin, small-framed body
* Lack of exercise, especially weight-bearing ones, such as walking and dancing
* Long-term bed rest
* Low calcium and vitamin D intake or absorption
* Smoking
* Drinking too much alcohol
* Long term use of some medicines, such as oral corticosteroids and antacids with aluminum
* Having certain health problems, such as anorexia nervosa, an over-active thyroid gland, and rheumatoid arthritis. Persons with Crohn’s disease, ulcerative colitis, and celiac disease are at an increased risk, too.
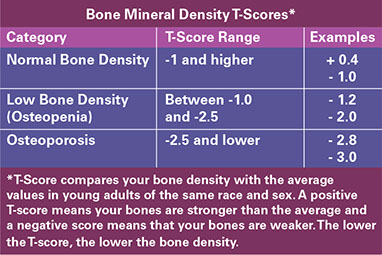
Diagnosis
There is no cure for osteoporosis. The focus is to:
* Prevent the disease
* Prevent further bone loss
* Build new bone
* All women 65 years of age and older should have a bone mineral density (BMD) screening test. Women who have had a fracture or are at a high risk for osteoporosis should get this test sooner than age 65, as advised by their doctors.
* Older men should have a BMD test if they have key risk factors for BMD-related fractures:
– A past fracture, possibly due to osteoporosis
– Low body weight. Physical inactivity.
– Prolonged use of corticosteroid medications.
{Note: Follow your doctor’s advice for when and how often to get screening tests for osteoporosis.}
* The most common test used to measure how dense bones are is a special X-ray known as a DXA or DEXA scan. You lie on a table and a technician moves a scanner above your spine, hip, or wrist. This safe and painless test takes about 10-20 minutes. Test results can identify persons who are at the highest risk for fractures.
Medical Care
Talk about your bone health with your doctor. Discuss:
* Your personal and family medical history
* Medications you take and have taken
* Falls or broken bones you have had as an adult
* Self-Care / Prevention measures you do already and ones you need help with
Medical treatment may include:
* Treatment for problems that increase the risk for low bone mass and osteoporosis
* Evaluating your risk of falls. Tests for this include ones that check your balance, vision, blood pressure, muscle strength, and heart rhythm.
* An exercise program for your needs. Physical therapy may be prescribed.
* High doses of vitamin D if your blood level is very low. Your doctor needs to prescribe this.
* Medications:
– Some slow down the breakdown of old bone. Two categories of these are bisphosphonates (biss-FOSS-fuh-nates) and anti-resorptive agents. Some of these medications are pills. Others are given in shots or through an IV.
– Another one (teriparatide) helps the body make new bone faster than the old bone is broken down.
Talk to your doctor about the benefits and risks of medications. Find out what side effects you should let him or her know about.
Reasons to Contact Doctor/Provider
* You have any “Signs & Symptoms” of Osteoporosis.
* You want to find out about medicines and other ways to prevent and/or treat osteoporosis.
* You are a female age 65 or older and have not had a bone mineral density (BMD) test.
* You are a female age 50 and older; you have had a fracture or are at high risk for osteoporosis; and you have not had a BMD test.
* You are an elderly male; you have risk factors for osteoporosis; and you need advice on getting a BMD test.
* After a fall, bump or strain, you have wrist, hip, or back pain.
* After a fall, you are not able to get up. Call or have someone call 9-1-1!
Self-Care / Prevention
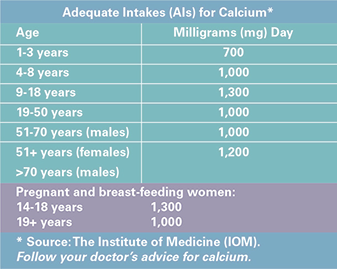
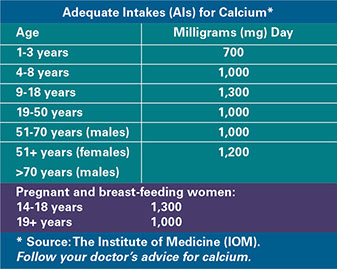
Get Your Recommended Adequate Intake (AI) for Calcium Every Day
* Choose high-calcium foods daily. Examples are milk, yogurt, salmon, and green leafy vegetables.
* Take calcium supplements, as advised by your doctor. It is best to limit calcium to 500 milligrams at a time. Ask your doctor about taking Tums® to get calcium.
* Eat a balanced diet. Have at least 5 fruits and vegetables every day. These have many vitamins, minerals, and anti-oxidants that can benefit bone health, as well as overall health.
* Don’t smoke. If you smoke, quit! Get help from your doctor,www.smokefree.gov, and/or 1.800.QUIT.NOW (784.8669).
* Limit alcohol. Too much alcohol interferes with the body’s need for calcium and vitamin D. It also increases the risk for falls.
* Take medications, as prescribed.
Sources of vitamin D:
* Sun exposure (without sunscreen) on your skin. Fifteen minutes of midday sunshine may meet the daily need. {Note: You may not get vitamin D benefits from the sun: During winter months; if you have dark skin; and/or you are age 60 years and older.}
* Foods, such as fortified milks and cereals, egg yolks, saltwater fish, and liver.
* Vitamin D supplements, as advised by your doctor. The best source of vitamin D for bone health is vitamin D3.
Use Fall Prevention Measures
(Falling is what leads to broken bones for many people with osteoporosis.)
* Ask your doctor if any medications you take could cause you to fall and how to deal with this. Find out how to deal with vision and balance problems, too.
* Put salt or kitty litter on icy sidewalks. Or stay home during bad weather!
* Use grab bars and safety mats, etc. in your tub and shower.
* Use handrails on both sides of stairways.
* When you reach for things on the floor or pick things up, bend at your knees, not at your waist.
* Wear flat, sturdy, nonskid shoes.
* If you use throw rugs, use ones with nonskid backs. Or tack them down to the floor.
* Use a cane or walker, if necessary.
* Keep halls, stairways, and entrances well lit. Use night lights in hallways, bathrooms, etc.
* Keep a flashlight next to your bed.
* Practice proper posture.
In the house, carry a cordless or cell phone with you, if you can. Doing this keeps you from rushing to answer the phone when it rings. You will also be able to call for help if you do fall.
Be Physically Active
Physical activity throughout life is important for bone health. Putting stress on your bones tells your body that your bones need to be made stronger.
* Do regular, weight-bearing exercise. Do this at least 3 or 4 times a week. Examples are walking, dancing, and step aerobics.*
* Do resistance exercises to strengthen muscles and build bone.* Examples are using weights and resistance bands.
* Do exercises that increase flexibility.* Examples are tai chi, yoga and stretching exercises.
* (Note: A person with osteoporosis should follow the exercise program outlined by his or her doctor.)
Low bone mass and osteoporosis pose a major health threat.
* One out of every 2 women and one in 4 men over age 50 will have an osteoporosis-related fracture in his or her lifetime.
* After a fracture, persons are more likely to have chronic pain, a fear of falling, and depression. They lose independence and have a lower quality of life.
* One year after a hip fracture, 1 in 4 people dies, 1 can’t walk, and 2 of the 4 can walk but are less mobile than before the fracture.
* In the U.S., costs for osteoporosis and related fractures have been estimated to be about $14 billion a year.
Resources
National Osteoporosis Foundation
800.231.4222
NIH Osteoporosis and Related Bone Disease National Resource Center
800.624.BONE (624.2663)