COVID-19 (COVID) is a disease caused by the SARS-CoV-2 virus. Most people recover within a few weeks. Older people and those with certain underlying medical conditions are more likely to become severely ill. Safe and effective vaccines are available to protect against COVID infections.
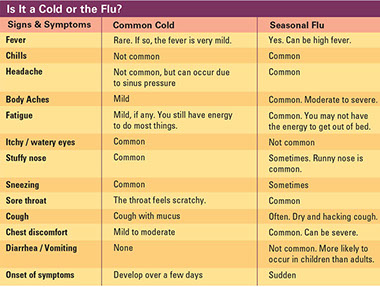
Signs & Symptoms
Symptoms may be mild or severe and appear 2-14 days after exposure to the virus. Symptoms may include:
* Fever or chills
* Cough
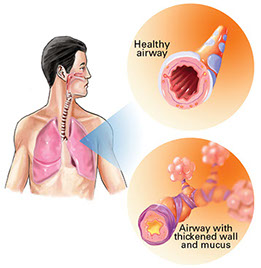
* Shortness of breath or difficulty breathing
* Fatigue
* Muscle or body aches
* Headache
* Loss of taste or smell
* Sore throat
* Congestion or runny nose
* Nausea or vomiting
* Diarrhea
Post-COVID conditions include a wide range of new, returning, or ongoing health problems for some people. They may occur four or more weeks after first being infected.
How COVID Spreads
* Breathing in air when close to an infected person who is breathing out air that contains the virus. People who are closer than 6 feet from the infected person are most likely to get infected.
* Having these virus particles from an infected person land on the eyes, nose, or mouth.
* Touching eyes, nose, or mouth with hands that have the virus on them.
Risk Factors for Severe Illness
Severe illness means needing hospitalization, intensive care, a ventilator to help breathe, or even death.
* Older people: The risk increases for people older than 50. People older than 85 are most likely to get very sick.
* People with certain underlying medical conditions: Examples include cancer, chronic kidney disease, and chronic lung disease, such as asthma, COPD, cystic fibrosis, and pulmonary hypertension. Others include dementia, diabetes, heart disease, HIV infection, weakened immune system, liver disease, overweight and obesity, sickle cell disease, smoking, and substance use disorders.
* Women who are pregnant.
Treatment
* Most people have mild illness from COVID and can recover at home.
* Get medical care immediately if you have trouble breathing or have any other emergency warning signs. Treatment may include medications and hospitalization to slow the virus, reduce an overactive immune response, support for the body’s immune function, or treat complications.
* One example of a medication used for treatment is monoclonal antibodies, which may help the immune system recognize and respond more effectively to the virus.
* Tell your close contacts that they may have been exposed to COVID so they can take precautions to protect their health, and the health of others close to them.
Prevention
Get vaccinated, including a booster shot, if recommended. This includes people who already had and not had COVID. These vaccines are safe and effective. They help protect against severe disease and death from variants of the virus. You may have side effects after vaccination, which is normal and should go away in a few days.
Use these following guidelines to help further prevent infection:
* Follow your local public health department’s recommendations to stay safe, especially if you live in or visit an area where there are high numbers of COVID cases.
* Follow guidelines issued by your workplace and local businesses.
* Wear a mask if you are not fully vaccinated when you are in indoor public places or crowded outdoor settings. You may also be recommended to avoid these areas.
* If you are fully vaccinated, you may also be recommended to wear a mask:
– When in areas of high numbers of cases
– If your age or an underlying medical conditions puts you at an increased risk for severe illness
– If someone in your household has a weakened immune system, is at increased risk for severe illness, or is unvaccinated.
* Wear a mask in planes, buses, trains, airports, stations, and ride-sharing services.
* Stay 6 feet away from others who do not live in your household. If possible, avoid close contact with people inside your household who are sick.
* Avoid indoor spaces that do not offer fresh air from the outdoors.
* Clean high touch surfaces regularly.
* Wash your hands often with soap and water for at least 20 seconds. Or use a hand sanitizer that contains at least 60% alcohol. This includes:
– Before eating or preparing food
– Before touching your face
– After using the restroom
– After leaving a public place
– After blowing your nose, coughing, or sneezing
– After handling your mask
– After changing a diaper
– After caring for someone who is sick
– After touching pets
* Cover coughs and sneezes. If wearing a mask, put on a new, clean mask as soon as possible. If you are not wearing a mask, cover your mouth and nose with a tissue, or the inside of your elbow.
* Limit the number of visitors and the time spent inside.
* Improve ventilation (air flow) in your home, especially when there are visitors. Open doors and windows if safe to do so. Filter the air in your home, using pleater furnace filters and change them every three months. Turn on bathroom and kitchen exhaust fans as well as other fans.
* Monitor your health daily. Be alert for symptoms, especially if you have been in a public setting and unable to keep a physical distance of 6 feet.
* If you have close contact with someone who has COVID, fully vaccinated people should wear a mask around others for 10 days and get tested at least 5 days after exposure. Unvaccinated people should quarantine. Stay home for 5 days, wear a mask around others and watch for symptoms. Get tested at least 5 days after exposure. If negative, you can leave your home but continue to wear a mask around others until 10 days after exposure. All people should get tested if they have symptoms.
Self-Care
* Stay home, except to get medical care. Stay in a specific room away from other people and pets in your household. Use a separate bathroom, if available.
* Monitor your symptoms carefully. Follow care instructions from your doctor and local health department.
* Your doctor may recommend taking medications, like acetaminophen or ibuprofen, to reduce fever. Other medications may also be recommended or prescribed that you can take while staying at home.
* Get rest and stay hydrated.
* Cover your mouth and nose with a tissue when you cough or sneeze. Immediately wash your hands.
* To find out where you can get tested, contact or visit the website of your local, state, or tribal health department.
* Wear a mask over your nose and mouth if you need to be around other people or animals, inside or outside your home.
* Wash your hands often with soap and water for at least 20 seconds. This includes:
– After blowing your nose, coughing or sneezing
– Going to the bathroom
– Before eating or preparing food
* If soap and water are not available, use hand sanitizer with at least 60% alcohol.
* Clean and disinfect high-touch surfaces every day in your “sick” room and bathroom. If other people clean these areas, they should wear a mask and disposable gloves.
* Do not share dishes, eating utensils, towels, or other bedding with other people in your home.