Women’s Health

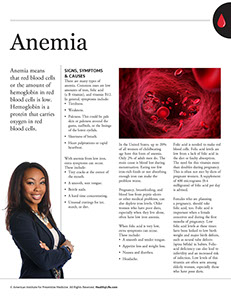
Anemia means that red blood cells or the amount of hemoglobin in red blood cells is low. Hemoglobin is a protein that carries oxygen in red blood cells.
Signs, Symptoms & Causes
There are many types of anemia. Common ones are low amounts of iron, folic acid (a B vitamin), and vitamin B12. In general, symptoms include:
* Tiredness.
* Weakness.
* Paleness. This could be pale skin or paleness around the gums, nailbeds, or the linings of the lower eyelids.
* Shortness of breath.
* Heart palpitations or rapid heartbeat.
With anemia from low iron, extra symptoms can occur. These include:
* Tiny cracks at the corner of the mouth.
* A smooth, sore tongue.
* Brittle nails.
* A hard time concentrating.
* Unusual cravings for ice, starch, or dirt.
In the United States, up to 20% of all women of childbearing age have this form of anemia. Only 2% of adult men do. The main cause is blood lost during menstruation. Eating too few iron-rich foods or not absorbing enough iron can make the problem worse.
Pregnancy, breastfeeding, and blood loss from peptic ulcers or other medical problems, can also deplete iron levels. Older women who have poor diets, especially when they live alone, often have low iron anemia.
When folic acid is very low, extra symptoms can occur. These include:
* A smooth and tender tongue.
* Appetite loss and weight loss.
* Nausea and diarrhea.
* Headache.
Folic acid is needed to make red blood cells. Folic acid levels are low from a lack of folic acid in the diet or faulty absorption. The need for this vitamin more than doubles during pregnancy. This is often not met by diets of pregnant women. A supplement of 400 micrograms (0.4 milligrams) of folic acid per day is advised.
Females who are planning a pregnancy, should take folic acid, too. Folic acid is important when a female conceives and during the first months of pregnancy. Low folic acid levels at these times have been linked to low birth weight and major birth defects, such as neural tube defects (spina bifida) in babies. Folic-acid deficiency can also lead to infertility and an increased risk of infection. Low levels of this vitamin are often seen among elderly women, especially those who have poor diets.
When vitamin B12 is low, extra symptoms can occur. These include:
* Chest pain on exertion.
* Swollen red tongue or bleeding gums.
* A hard time concentrating.
* Appetite loss and weight loss.
* Nausea and diarrhea.
When vitamin B12 is very low, nervous system problems can occur, such as:
* Numbness and tingling in the hands and feet.
* Walking and balance problems.
* Memory loss, confusion, dementia or psychosis.
One form of vitamin B12 deficiency anemia is pernicious anemia. This is usually caused when the body doesn’t absorb vitamin B12 from food. It can result from a lack of digestive acids and a substance called the intrinsic factor. Both are needed to absorb vitamin B12. Other causes are surgery that removes part or all of the stomach and autoimmune problems that cause cells in the stomach’s lining to shrink. Vitamin B12 is found only in animal foods. It is not in plant foods unless the vitamin is added, such as in some cereals.
Other Types of Anemia
* Sickle cell anemia. This is an inherited disorder that affects the red blood cells’ ability to carry oxygen to the body’s tissues. Sickle cell anemia occurs mostly in African Americans but can occur in other ethnic groups too.
* Aplastic anemia. This is a serious disease of decreased bone marrow production.
Also, alcohol, certain drugs, large amounts of aspirin, and some chronic diseases can cause anemia.
Treatment
Anemia shares symptoms with many health problems. It needs to be diagnosed by a doctor. Persons with severe anemia may need one or more blood transfusions.Treatment for it depends on the type and what caused it. This includes:
* Treating the problem that caused it.
* Eating a proper diet and taking vitamin and/or mineral supplements, as prescribed. {Note: Don’t take iron supplements on your own. Persons with a genetic illness called hemochromatosis (iron overload disease) can be harmed with iron supplements.}
* Getting vitamin B12 shots, if needed.
Questions to Ask
Self-Care
To Get and Absorb Iron
* Eat foods that are good sources of iron: green leafy vegetables, lean red meat, beef liver, poultry, fish, wheat germ, oysters, dried fruit, and iron-fortified cereals.
* Eat foods high in vitamin C, such as citrus fruits, kiwi, tomatoes, strawberries, broccoli, and green or red bell peppers.
* If you drink tea, drink it between meals. Tannins in tea block iron absorption. Or add milk to tea. The calcium in milk binds with the tannins. (Herbal tea does not have tannins.)
* Take the supplements your doctor advises. {Note: High levels of iron in the blood may increase the risk for heart attacks. This is especially a concern if you have gone through menopause.}
* Avoid antacids, phosphates (which are found in soft drinks, beer, ice cream, candy bars, etc.), and the food additive EDTA. These block iron absorption.
To Get and Absorb Folic Acid
* Eat good food sources of folate every day. These include asparagus, Brussels sprouts, spinach, romaine lettuce, collard greens, and broccoli. Other good sources are black-eyed peas, cantaloupe, orange juice, oatmeal, and whole-grain or fortified cereals.
* Eat fresh, raw fruits and vegetables often. Don’t overcook food. Heat destroys folic acid.
* Take the supplement your doctor advises.
* Don’t smoke or drink alcohol.
Tips for Getting Vitamin B12
* Eat animal sources of food. Good choices are lean meats, fish, poultry, nonfat or low-fat dairy products.
* Strict vegetarians (vegans) who eat no animal sources of food should get vitamin B12 from a supplement or foods fortified with it, such as cereals or plant-based milks or nutritional yeast.
Resources
National Heart, Lung, and Blood Institute