Nutrition
Cholesterol is a waxy, fat-like substance. It occurs naturally in the body. It helps carry fat through your blood vessels.
What is Cholesterol?
Your body also needs cholesterol to:
* Make cell walls
* Make vitamin D and some hormones
* Give structure to the covering (myelin) that protects nerve fibers
* Make bile. This helps your body digest fat.
Your body only needs a small amount of cholesterol in your blood to meet these needs.
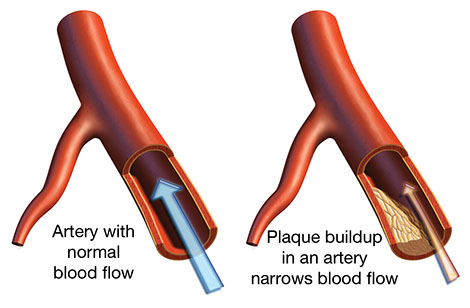
Too much cholesterol in your blood can collect with other fats and calcium to make plaque. This can clog the walls of the arteries and slow down or block blood flow to the heart or brain. The higher your blood cholesterol, the greater your chance of this buildup.
Where Does Cholesterol Come From?
* Cholesterol the body makes (mostly in the liver)
* Cholesterol in animal foods (dietary cholesterol)
Plants do not have cholesterol. Some plant foods have saturated and trans fat (hydrogenated oils) which raise blood cholesterol.
Cholesterol Test
A “lipoprotein profile” blood test checks your blood cholesterol (lipid) numbers. For accurate results, do not eat or drink anything, except water, for 9-12 hours before the test. A non-fasting test can screen for total and HDL-cholesterol levels.
Who should get a blood cholesterol test?
* All men age 35 and older
* Men ages 20-35 and women age 45 and older who are at an increased risk for coronary artery disease
* Persons with diabetes and/or heart disease
Get tested as often as advised by your doctor.
What Should Your Cholesterol Numbers Be?
For cholesterol to travel through blood, it is coated with a protein. This makes a “lipoprotein.” Total blood cholesterol is made up of these lipoproteins:
* LDL (low density lipoprotein) cholesterol
* HDL (high density lipoprotein) cholesterol
* VLDL (very low density lipoprotein) cholesterol.
*Note: Your doctor will discuss and prescribe treatment and medication based on your target blood cholesterol numbers, plus other risk factors:
* Your age and health conditions, such as diabetes and cardiovascular disease (CVD)
* Your LDL-cholesterol and 10-year risk for CVD
* A family history of premature CVD
* Other CVD risk factors
Heart Disease Risk Factors
Remember, blood cholesterol is only one risk factor for cardiovascular disease. Others are include:
* You have had a heart attack or stroke.
* Cigarette smoking. Secondhand smoke.
* High blood pressure
* High LDL-cholesterol level
* Diabetes or insulin resistance
* Being overweight or obese.
* Lack of exercise.
* Sleep apnea.
* Being male 45 years+ or female 55 years+
* Heart disease in a father or brother before age 55; in a mother or sister before age 65
* Kidney disease
* Excess alcohol
* Stress, often with anger, can trigger a heart attack.
* Metabolic syndrome.
– Waist size ≥ 40 inches for men; ≥ 35 inches for women
– Blood pressure ≥ 130 mm Hg systolic and/or ≥ 85 mm Hg diastotic or you take medicine to lower blood pressure
– A fasting blood sugar ≥ 100 mg/dL or you have diabetes
– Triglycerides ≥ 150 mg/dL
– HDL-cholesterol < 40 mg/dL for men; < 50 mg/dL for women.
Eat Healthy
* Choose foods low in saturated fat and with zero trans fat. These raise LDL (bad) cholesterol in the blood more than anything else in the diet. Read food labels. Trans fats are in foods that have hydrogenated oils.
* Eat foods with plant sterols and stanols, such as margarines and salad dressings made with these.
* Choose monounsaturated and polyunsaturated fats.
* Limit meat serving sizes. Choose lean cuts of beef, pork and lamb. Trim fat from meat. Choose chicken and turkey. Take the skin off poultry before you eat it.
* Eat fish 2 to 3 times a week (e.g., salmon). Fish has omega-3 fatty acids, a healthy unsaturated fat. So does cod liver oil. Ask your doctor about fish oil supplements. Find out about mercury and other pollutants in fish fromwww.epa.gov.
* Get 20 to 35 grams of dietary fiber a day, especially the water-soluble type from oat bran, oatmeal, kidney and other beans, lentils, apples, oranges, and carrots.
* Eat a variety of whole-grain breads, cereals, and pastas; fruits and vegetables; lentils; beans, etc. These plant foods are low in saturated fat and have no cholesterol (if you do not add fatty toppings and spreads). Have soy milk, soy yogurt, and tofu.
* Limit alcohol to 2 drinks a day for men and 1 drink a day for women and persons age 65 and older. One drink = 4 to 5 oz. of wine, 12 oz. of beer, or 1-1/2 oz. of 80 proof liquor (whiskey, vodka, etc.).
* Your doctor may tell you to limit dietary cholesterol to 300 milligrams (mg) a day (200 mg a day if your cholesterol is high).
Prescribed Medicines
Your doctor may prescribe cholesterol-lowering medication. This is used with, not instead of, life style changes.
Types of Cholesterol-Lowering Medicines
* Statins. These help your body make less cholesterol and help the liver remove LDL (bad) cholesterol already in the blood. Examples are lovastatin and pravastatin. Statins lower LDL (bad)cholesterol more than any other type of drugs. They also lower triglycerides and raise HDL (good) cholesterol.
* Resins. These bind with cholesterol-containing bile acids in the intestines and are then passed in the stool. Examples are cholestyramine and colestipol. These lower LDL (bad) cholesterol.
* Nicotinic Acid or Niacin. This is a B vitamin. You can buy this over-the-counter, but a doctor should prescribe the amount you take and monitor its use. Niacin lowers LDL (bad) cholesterol and triglycerides and raises HDL (good) cholesterol.
* Fibrates. These medicines lower triglycerides and raise HDL (good) cholesterol. Examples are gemfibrozil and fenofibrate.
Tips On Taking Your Medication
* Take your medication as prescribed. If you have questions, talk to your doctor or pharmacist.
* Tell your doctor about side effects. Common side effects with many cholesterol-lowering medicines are bloating, gas, abdominal pain, constipation, and nausea. Hot flashes or flushing is common with niacin. Ask your doctor how to minimize these side effects. Often they wane with time. Make sure to tell your doctor if you have muscle soreness or weakness, and/or brown urine.
Resources
American Heart Association
800.AHA.USA1 (242.8721)
National Heart, Lung, and Blood Institute
