Women’s Health
For Breast Lumps
Feeling a lump in a breast can be scary. For a lot of women, the first thought is cancer. The good news is that 80% to 90% of breast lumps are not cancer.
Signs, Symptoms, and Causes
* Solid tumors. These include:
– Lipomas. These are fatty tumors that can grow very large. They are usually benign.
– Fibroadenomas. These lumps are round, solid, and movable and are usually benign.
– Cancerous lumps. Often, these are firm to hard masses that do not move when felt. They are often an irregular shape.
* Cysts. (These can be very small and diffuse, as in fibrocystic breast disease). These cysts:
– Are fluid filled sacs.
– Are painful and feel lumpy or tender.
– Can occur near the surface of the skin of the breast and/or be deep within the breast. This second type may need to be tested with a biopsy to make sure it is benign.
* Nipple-duct tumors. These tumors occur within the part of the nipple that milk flows through. They cause a discharge from the nipple. These tumors should be removed by surgery.
* In rare cases, a bloody discharge from the nipple could be a sign of cancer.
Treatment
Tests can be done to help diagnose whether or not a breast lump is benign.
* Mammogram. This X-ray of the breast can detect breast problems before they can be felt.
* Ultrasound. This tells whether the lump is fluid-filled (usually harmless) or solid.
* Needle aspiration. With this, a needle is put into the lump to remove fluid or cells.
* Biopsy. There are many types. With these, a sample of the breast tissue is taken and examined.
* Ductal lavage. Fluid is sent through a catheter to the milk ducts. Cells inside the milk ducts are collected and checked for the risk of breast cancer.
Benign breast lumps may go away if you breast-feed for many months or take a low-dose birth control pill. Prescribed medicines can get rid of severe breast lumps. These have side effects, though.
For Breast Cancer
Signs & Symptoms
Breast cancer is the most common form of cancer among women. It accounts for 30% of cancers women get. Each year, there are about 227,000 new cases of breast cancer. About 49,500 women die from it. Only lung cancer causes more cancer deaths among women.
Breast cancer often develops without signs and symptoms. This is why screening for breast cancer is needed.
Causes & Risk Factors
Breast cancer results from malignant tumors that invade and destroy normal tissue. When these tumors break away and spread to other parts of the body, it is called metastasis. Breast cancer can spread to the lymph nodes, lungs, liver, bone, and brain.
* Being a women is the main risk factor. {Note: Men can get breast cancer, too. Yearly, about 410 men die from breast cancer. Men should look for and report a breast lump or other change to their doctors.}
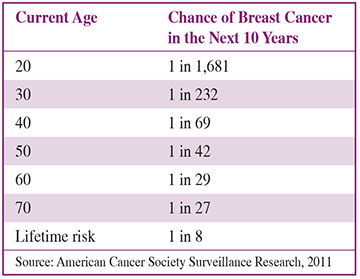
* Increase in age. The American Cancer Society has given these figures for women’s chances of getting breast cancer:
* Changes in BRCA1, BRCA2, and other cancer genes.
* Personal history of breast cancer.
* A mother or sister has or had breast cancer.
* One or more breast biopsies were done, especially if they showed certain changes in breast tissue.
* Dense breast tissue (shown on mammograms).
* Radiation therapy to the chest before age 30.
* Never giving birth or having a first full-term pregnancy after age 30. Never breast-fed a child.
* Menstruation started before age 12. Menopause occurred after age 55.
* Hormone therapy (estrogen plus progestin) after menopause and/or recent use of birth control pills may be factors.
* Being overweight or obese after menopause.
* Alcohol. The more consumed, the higher the risk.
* Race. Caucasian women have a slightly greater risk than African American, Asian, Hispanic, and Native American women.
* Eastern and Central European Jewish ancestry.
* Lack of physical activity throughout life.
Ask your doctor about your risk for breast cancer. Contact the National Cancer Institute for The Breast Cancer Risk Assessment Tool. Accesswww.cancer.gov/bcrisktoolor call 800.4.CANCER (422.6237).
Detection
* Breast exams by a doctor or nurse and mammograms. Have mammograms at facilities that are accredited by the American College of Radiology (ACR). Call The National Cancer Institute 800.4.CANCER (422.6237) to find ones in your area.
* Ultrasound exam.
* Magnetic resonance imaging (MRI).
* Noticing problems in your breasts.
If you find a change in a breast or a lump, call your doctor. Additional tests can check for cancer. Most lumps that are found and tested are not cancer.
Treatment
Finding and treating the cancer early is vital. Treatment is based on the type, size, and location of the tumor. It also depends on the stage of the disease and individual factors you may have.
One or More of These Treatment Methods are Used
* Surgery.
* Sentinal lymph node biopsy and surgery.
* Chemotherapy.
* Radiation therapy.
* Targeted therapy. This kills cancer cells but not normal cells.
* Hormone therapies.
* Stem cell or bone marrow transplant.
* Clinical trials.
Questions to Ask
Self-Care / Prevention
For Cystic Breasts
* Get to and stay at a healthy body weight.
* Follow a low saturated fat diet. Eat soy foods.
* Do regular exercise. This can promote blood flow to your breasts.
* Limit or have no caffeine.
* Limit salt and sodium intake. This helps prevent fluid buildup in the breasts.
* Don’t smoke. Don’t use nicotine gum or patches.
* Take an over-the-counter pain reliever.
* Take vitamin E, as advised by your doctor.
* Wear a bra that provides good support. You may want to wear it while you sleep, too.
For Breast Pain and/or Swelling without Lesions or Redness
* For pain due to trauma or surgery, apply cold packs for the first 48 hours. Do this every 2 to 4 hours for 10 to 15 minutes at a time. After 48 hours, apply heat, such as a hot water bottle. Do this 4 times a day for 10 to 15 minutes at a time.
* For pain not due to trauma or injury, apply warm heat. Use a heating pad set on low or a hot water bottle. Do this for 30 minutes. Then apply an ice pack for 10 minutes. Repeat as often as needed.
* Take vitamins, as advised by your doctor.
* Take an over-the-counter medicine for pain and swelling, as directed.
To Reduce the Risk for Breast Cancer
* If you are at a high risk for breast cancer, ask your doctor about taking prescribed medicine, such as raloxifene.
* Avoid X-rays that are not needed. Wear a lead apron when you get dental and other X-rays not of the chest.
* Eat a variety of fruits and vegetables and whole-grain breads and cereals.
* Get to and stay at a healthy body weight.
* Do 30 or more minutes of moderate activity most days of the week. Daily is better.
* Limit alcohol intake to 1 drink per day, if any.
* Breast-feed your babies.
Breast Self-Exam
Breast observance is being aware of how your breasts normally look and feel and checking for changes. You can do this while you shower or get dressed. A breast self-exam (BSE) is a step-by-step method to examine your breasts. Beginning at age 20, ask your health care provider about the pros and cons of doing a BSE. If you choose to do a BSE, use the steps given on this page. At your next health exam, show your health care provider how you do a BSE.
BSE Steps
Examine your breasts during times of the month when they are not normally tender or swollen. For example, if you menstruate, the best time may be within 3 days after your period stops.
1. Lie down. Place a pillow under your right shoulder and put your right hand behind your head.
2. Move the pads of your left hand’s 3 middle fingers, held flat, in small, circular motions as you start to feel your right breast tissue.
3. Use this circular motion in an up and down pattern as you check the entire breast area. This includes the area from as high up as your collarbone to as low as the ribs below your breast; and from your right side (imagine a line straight down from under your arm) across the breast to the middle of your chest bone.
Feel every part of the entire area you check with 3 different levels of pressure:
* Light – Feel the tissue closest to the skin.
* Medium – Feel a little deeper than the skin.
* Firm- Feel the tissue closest to your chest and ribs.
4. Squeeze the nipple gently. Check for a clear or bloody discharge.
5. Repeat steps 1 to 4 for the left breast using the finger pads of your right hand.
6. Stand in front of a mirror. Press your hands firmly on your hips. Look for:
– Any changes in the size, shape, or contour of your breasts
– Puckering, scaling, or redness of the skin
– Nipple changes or discharge
7. Sit or stand. Raise your arm slightly. Examine each underarm area for lumps or changes.
If you a find a lump or any change in the way your breasts normally look or feel, let your health care provider know right away. Most lumps that are found and tested are not cancer.
Resources
National Cancer Institute
800.4.CANCER (422.6237)
National Breast and Cervical Cancer Early Detection Program (NBCCEDP)
800.CDC.INFO (232.4636)