First Aid
A heart attack happens when the heart does not get enough blood supply for a period of time. Part or all of the heart muscle dies.
Signs, Symptoms & Causes

A heart attack may have warning signs. It can occur without signs, too. This is called a “silent” heart attack.
Causes
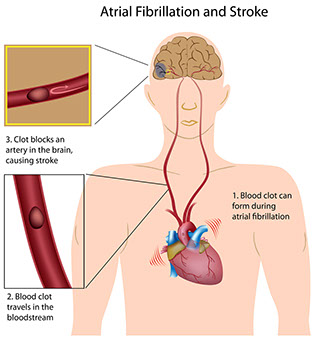
* The most common cause is one or more blood clots that block an artery in the heart. Often, a blood clot forms in an artery already narrowed by plaque.
* Having a heart attack in the past increases the risk for another one.
* Spasms occur in the large coronary artery. This can be triggered by: Heavy physical exertion, such as shoveling snow; exposure to cold; severe emotional stress; and having a heavy meal. These triggers are more likely to affect persons who are not active.
* Cocaine or amphetamine abuse can cause a sudden heart attack. This can happen in persons with no signs of heart disease.
Warning Signs
Note: If any of these signs occur, call 9-1-1.
Common Warning Signs
* Feeling of pain (may spread to or be felt in the arm, neck, tooth, jaw, or back), tightness, burning, squeezing, or heaviness in the chest. This lasts more than a few minutes or goes away and comes back.
* Chest discomfort with:
– Fainting
– Feeling lightheaded.
– Nausea.
– Shortness of breath.
– Sweating.
Other Warning Signs
* Unusual chest, abdominal, or stomach pain.
* Dizziness; nausea; trouble breathing; jaw or arm pain without chest pain.
* Fast or uneven heartbeat or pulse.
* Sweating for no reason, pale, gray, or clammy skin.
Signs More Likely in Women Than Men
An uneasy feeling in the chest with: Unexplained or extreme anxiety; unusual fatigue or weakness; fluttering heartbeats; or severe indigestion that doesn’t go away with an antacid.
Treatment
A heart attack is a medical emergency! Treatment works best when it is given within 1 to 2 hours after symptoms start. Treatment includes:
* Medicine(s) to keep blood from clotting.
* “Clot busters” to dissolve blood clots in heart arteries.
* Tests to diagnose the status of the heart and arteries.
* Angioplasty, stents, or bypass surgery, if needed.
Prevention
* Follow prevention measures in Heart Disease.
* Take medications, as prescribed.
* Don’t shovel snow or carry heavy objects, especially if you are not physically fit.
* Don’t use amphetamines and/or cocaine.
Questions to Ask
Self-Care / Prevention
Call 9-1-1 or your local rescue squad right away! Call when warning signs start. Don’t wait to see if the pain goes away.
First Aid for a Heart Attack Before Emergency Care
* CHECK for a response. Do CPR, as needed.
* If the person uses and has nitroglycerin, place one tablet under the tongue. Give as many as 3 tablets in 10 minutes.
* Give the person a regular (325 mg.) aspirin or 4 children’s chewable aspirins (81 mg. each) to chew on. Give the aspirin after calling 9-1-1. Ask the 9-1-1 dispatcher if aspirin should be taken.
{Note: Don’t use aspirin if the person is allergic to it or has a condition that makes using it risky.}
* If you can’t call 9-1-1, drive the person to the hospital right away. If you are having heart attack signs, don’t drive yourself unless you have no other choice.
* Loosen clothing around the neck, chest, and waist. Don’t let the person lie down, especially if he or she has breathing problems. A half-sitting position is better. Put the legs up. Bend them at the knees. Put a pillow or rolled towel under the knees. Support the back.
* Reassure the person that you have called for medical help and will stay with him or her until it arrives.
* After a heart attack, follow the doctor’s treatment plan.