SELF-CARE CORNER
If you wear glasses or contacts, it’s possible you may be a candidate for LASIK eye surgery. LASIK stands for laser-assisted in situ keratomileusis, which simply means laser vision correction.
The procedure uses a laser to correct the shape of your cornea and improve your vision. This type of surgery is used to treat:
* Myopia (nearsightedness)
* Hyperopia (farsightedness)
* Astigmatism (an imperfection in the shape of the cornea)
Undergoing LASIK eye surgery may reduce or eliminate your need for glasses or contacts. But, it’s not right for everyone.
How to qualify
To find out if you are a candidate for LASIK, you first need to talk to your eye doctor. They will do a comprehensive eye exam and make sure you meet certain criteria such as:
* Stable vision for at least a year
* Eye prescription within the range LASIK can correct
* Thick healthy corneas
* 18 years of age or older
Some conditions may disqualify you from the procedure. These include:
* Severe dry eye
* Eye infections
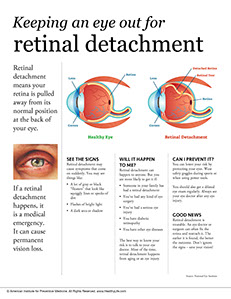
* Cataracts
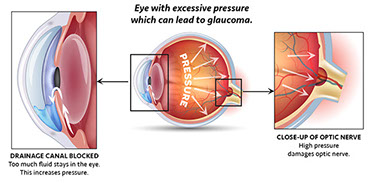
* Glaucoma
* Poorly controlled diabetes
* Pregnancy or breastfeeding
The procedure
During the procedure, you will be awake, resting comfortably on a table, and able to see for the majority of the time. It is painless and over in just a few minutes.
1. Drops will be put in your eyes to numb them.
2. An eyelid holder will be put in place to keep your eyes open.
3. A suction ring will be placed on your eye to hold it still. You will feel some pressure, and your vision will briefly fade.
4. The ophthalmologist will use a laser to cut a flap in your cornea.
5. A laser will precisely reshape your cornea, and the flap will be smoothed back into place.
After LASIK surgery
You will need to wear special glasses at first for eye protection and use several types of eye drops for the first few days to weeks until your eyes are healed.
Side effects from the procedure are often temporary and may include:
* Dry eyes
* Light sensitivity
* Blurry vision
* Halos around lights, especially at night
* Glare
Source: American Academy of Ophthalmology