First Aid
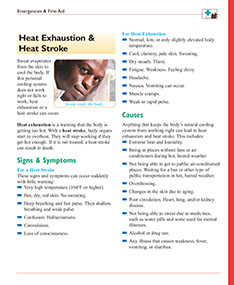
Signs & Symptoms
For a Severe Injury
* The scalp, neck, or back bleeds.
* It looks like the head, neck, or back is in an odd position.
* Pain is felt in the back, neck, and/or head. The pain can be severe.
* Stiff neck.
* Abdominal pain. Vomiting.
* Blood or fluid comes from the mouth, nose, or an ear.
* Loss of vision. Blurred or double vision. Pupils of uneven size.
* Inability to move any part of the body. Weakness in an arm or leg. Walking is difficult.
* New feelings of numbness occur in the legs, arms, shoulders, or any other part of the body.
* New loss of bladder or bowel control occurs.
* Confusion. Drowsiness. Personality changes.
* Convulsions.
* Loss of consciousness.
Watch for signs and symptoms for the first 24 hours after the injury. Symptoms may not occur for as long as several weeks, though. Problems can occur even if no injury is seen on the outside.
For a Whiplash Injury
* Neck pain and stiffness.
* Having a hard time raising the head off of a pillow.
Causes
Anything that puts too much pressure or force on the head, neck, or back can result in injury. Common causes are falls, accidents, and hard blows. A concussion occurs when the brain is shaken. A contusion occurs when the brain is bruised.
Treatment
If you suspect a head, neck, or back injury, you must keep the head, neck, and back perfectly still until EMS arrives. Any movement of the head, neck, or back could result in paralysis or death.
Questions to Ask
Self-Care / Prevention
First Aid for a Severe Injury
* Do not move the person unless his or her life is in danger. If so, log roll the person, place tape across the forehead, and secure the person to a board to keep the head, neck, and back areas from moving at all.
* Call 9-1-1!
* CHECK for a response. If giving rescue breaths, do not tilt the head backward. Pull the lower jaw open instead.
To Immobilize the Head, Neck, and/or Back
* Tell the person to lie still and not move his or her head, neck, back, etc.
* Log roll as listed above or place rolled towels, etc. on both sides of the neck and/or body. Tie in place, but don’t interfere with the person’s breathing. If necessary, use both of your hands, one on each side of the person’s head to keep the head from moving.
* Monitor for Bleeding and Shock. Keep the person warm with blankets, coats, etc.
Move Someone You Suspect Has Injured His or Her Neck in a Diving or Other Water Accident
Before emergency care arrives:
* Protect the neck and/or spine from bending or twisting. Place your hands on both sides of the neck. Keep it in place until help arrives.
* If the person is still in the water, help the person float until a rigid board can be slipped under the head and body, at least as far down as the buttocks.
* If no board is available, get several people to take the person out of the water. Support the head and body as one unit. Make sure the head does not rotate or bend in any way.
First Aid For Traffic Accidents
* If the person was in a motorcycle accident, do not remove the helmet. Call 9-1-1 to do this.
* Don’t move the person. He or she may have a spinal injury. Call 9-1-1 to do this.
First Aid for Minor Head Injuries
* Put an ice pack or bag of frozen vegetables in a cloth. Apply this to the injured area. Doing this helps reduce swelling and bruising. Change it every 15 to 20 minutes for 1 to 2 hours. Do not put ice directly on the skin. Cover an open, small cut with gauze and first- aid tape or an adhesive bandage.
* Once you know there is no serious head injury, do normal activities again. Avoid strenuous ones.
* Take an over-the-counter medicine for pain as directed.
* Don’t drink alcohol or take any other sedatives or sleeping pills.
* During the next 24 hours, monitor the person. While asleep, wake the person every 2 hours to check alertness. Ask something the person should know, such as a pet’s name, an address, etc. If the person can’t be roused or respond normally, get immediate medical care.
First Aid for Bleeding from the Scalp
* To control bleeding, put pressure around the edges of the wound. Make a ring pad (shaped like a doughnut) out of long strips of cloth to apply pressure around the edges of the wound. If this doesn’t control bleeding, put direct pressure on the wound. Don’t poke your hand into the person’s brain, though.
* Don’t wash the wound or apply an antiseptic or any other fluid to it.
* If blood or pink-colored fluid is coming from the ear, nose, or mouth, let it drain. Do not try to stop its flow.
If You Suspect a Whiplash Injury
* See your doctor, as soon as you can, to find out the extent of injury. If your arm or hand is numb, tell your doctor.
* For the first 24 hours, apply ice packs to the injured area for up to 20 minutes every hour.
* After 24 hours, use ice packs or heat, whichever works best, to relieve the pain. There are many ways to apply heat. Take a hot shower for 20 minutes a few times a day. Use a hot-water bottle, heating pad (set on low), or heat lamp directed to the neck for 10 minutes, several times a day. (Use caution not to burn the skin.)
* Wrap a folded towel around the neck to help hold the head in one position during the night.
Concussion
This is a mild traumatic brain injury (TBI) from a blow or jolt to the head. Signs and symptoms are:
* Altered level of alertness. May have brief fainting spell. Feeling confused, dazed, and/or dizzy.
* Can’t remember events right before or right after the injury.
* Nausea and vomiting.
* Headache.
A concussion needs a medical assessment.