MEDICAL NEWS

Medications improve the quality of life for many people. When you have a medical condition, the right medication can make all the difference.
Polypharmacy refers to the use of multiple medications, generally in the range of 5-10 each day. It is common in older adults; however, anyone who struggles with more than one chronic condition may be at risk.
While taking medication to protect your health is essential, you should be aware of the danger associated with polypharmacy and how to prevent it.
The danger of polypharmacy
Every drug is studied to make sure it is safe and effective to treat the condition it is used for. But, once you start mixing multiple medications together, the side effects may be less known and hard to predict.
Anyone taking more than five medications is at risk for:
* Adverse drug reactions
* Balance issues
* Cognitive impairment
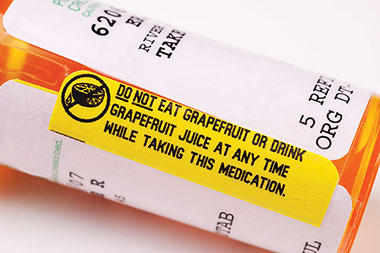
* Harmful drug interactions
* Drug-disease interactions
Taking a lot of different medications also creates a burden on you, the patient, to manage and keep track of everything you are taking.
Ways to decrease your risk
* Keep an updated list of all your medications. Take it with you to every doctor’s appointment. If you see multiple doctors, this is especially critical.
* Talk to the pharmacist every time you are prescribed a new medication. Make sure to show them your medication list so they can check for any drug interactions.
* If possible, fill all your prescriptions at one pharmacy.
* Don’t stop taking a medication on your own. Always talk to your doctor if you are concerned about the amount of medicine you are taking.
Questions to ask your doctor
Your doctor is your best resource to decrease your risk of polypharmacy. Always review your medications with them at each visit and ask detailed questions. Here are some questions to ask:
* Is there one medication that could help with multiple conditions?
* Do the benefits of the drug outweigh the risks?
* Should I keep taking a medicine that doesn’t seem to be working?
* Can the dosage be adjusted to decrease the risk of side effects?
* Could a new symptom be a side effect of my medication?