Pregnancy & Prenatal Care
Causes
Pregnant women get backaches because:
* The growing uterus and extra weight pull the body forward. Standing this way can strain the back muscles.
* Hormones are released during pregnancy. These make the ligaments soften and stretch. Ligaments are tissues that surround and support the joints.
* Joints in the lower back get sore from pressure. This happens to joints in the pelvic area, too. The baby is growing in size and weight.
* The baby presses against the tailbone.
Prevention
Do exercises your health care provider tells you to do. Use good posture, too. Keep your spine straight when you are standing. Have a friend check your back for curving: Stand with your heels against a wall. Ask your friend to look at your back. Tell him or her to let you know if it curves. Center your weight over the pelvic area. Be careful when you bend over, too. Bending wrong can give you a backache.
Back Labor
Most women have some back pain during labor. Some women have it through their whole labor. This is called back labor. It is caused by the way the baby is lying. The back of the baby’s head presses against the tailbone. Or it may press slightly to one side of it. Back labor can occur in preterm labor, too.
Questions to Ask
Self-Care
Tips for Good Posture
When you stand:
* Stand straight.
* Tuck in your bottom.
* Don’t hollow your back.
* Don’t tighten your shoulders or hold them back. Keep them dropped.
* If you have to stand for a long time: Stretch your feet and shift your weight. Rest one foot and then the other on a footstool or telephone book.
When you sit:
* Sit on a straight chair with a high back.
* Rest your back against the chair’s back.
* Put a pillow at the small of your back.
* Rest one or both feet on a footstool.
* Don’t sit too long. It strains your lower back. Get up and walk around.
When you bend:
* To pick something up, squat down on your heels and bend your knees. Keep your upper body straight. Don’t lean over from the waist. Use the strength from your legs, not your back.
* To do something down low, kneel or squat. Or get down on all fours. That way, you help take the baby’s weight off your spine.
When you lie down or sleep:
* Use a firm mattress. If you don’t have one, have someone help you place a board under your mattress. Or have someone put your mattress on the floor.
* Lie on your left side with your knees bent. Bend the upper knee more than the lower knee. Leave a lot of space between your legs.
* Put a pillow under your upper knee and leg.
Other Self-Care Tips
* Don’t gain too much weight.
* Wear shoes with low (but not flat) heels.
* On a long car ride, stop every two hours. Get out and walk around.
* Don’t take medicine for pain. Ask your health care provider first.
* Don’t lift objects over 15 pounds.
* Don’t do exercises where you lift both legs at the same time.
* Do exercises for stronger back and belly muscles. Ask your health care provider for these.
* Do relaxation and deep breathing exercises. Do yoga.
* Have someone massage your lower back. Massage won’t cure a backache. It can loosen tight muscles, though.
* Apply warm, moist heat to your back. Use a hot water bottle or warm wash cloth.
* Ask your health care provider if you should wear a back support girdle, a back brace, or a special elastic sling.
* Do an exercise called the “pelvic rock”. This exercise helps your lower back be more flexible. It helps make the muscles in your belly stronger.
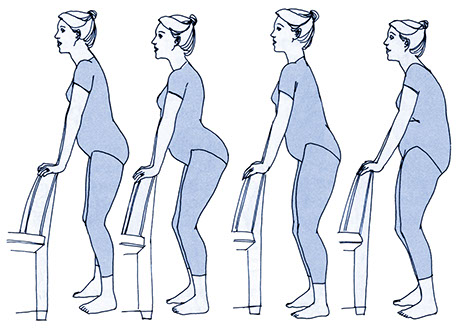
You can stand to do the pelvic rock.
Step 1
* Stand 2 feet away from the back of a chair.
* Put your hands on the chair’s back. Keep your elbows straight.
* Bend a little forward from your hips.
Step 2
* Push your hips backward and relax the muscles in your belly. Relax your back.
* Bend your knees a little.
Step 3
* Slowly pull your hips forward.
* Tuck your buttocks under as if someone were pushing you from behind.
Step 4
* Repeat steps 1, 2, and 3.
You can do the pelvic rock on your hands and knees.
Step 1
Get down on all fours. Have your knees slightly apart. Have your back and elbows straight.
Step 2
Breathe in. As you breathe in, relax your back. Use the muscles in your lower belly.
Step 3
Breathe out. As you breath out, let your back relax down to a flat position. Do not let your back sag.
Step 4
Repeat steps 1, 2, and 3.
{Note: Tell your health care provider if you get pain when you do the pelvic rock. Ask for help if you have a problem doing the pelvic rock.}