SELF-CARE CORNER

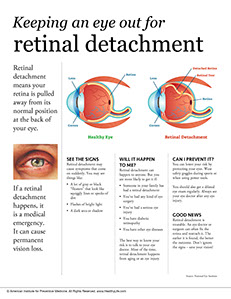
Retinal detachment means your retina is pulled away from its normal position at the back of your eye. If a retinal detachment happens, it is a medical emergency. It can cause permanent vision loss.
See the signs
Retinal detachment may cause symptoms that come on suddenly. You may see things like:
* A lot of gray or black “floaters” that look like squiggly lines or specks of dirt
* Flashes of bright light
* A dark area or shadow
Will it happen to me?
Retinal detachment can happen to anyone. But you are more likely to get it if:
* Someone in your family has had a retinal detachment
* You’ve had any kind of eye surgery
* You’ve had a serious eye injury
* You have diabetic retinopathy
* You have other eye diseases
The best way to know your risk is to talk to your eye doctor. Most of the time, retinal detachment happens from aging or an eye injury.
Can I prevent it?
You can lower your risk by protecting your eyes. Wear safety goggles during sports or when using power tools.
You should also get a dilated eye exam regularly. Always see your eye doctor after any eye injury.
Good news
Retinal detachment is treatable. An eye doctor or surgeon can often fix the retina and reattach it. The earlier it is found, the better the outcome. Don’t ignore the signs – save your vision!
Source: National Eye Institute