Substance Use & Abuse
After alcohol, the most common drugs used are tobacco and marijuana. Other drugs used are amphetamines (uppers); barbiturates (downers); hallucinogens, such as LSD; inhalants; and narcotics, such as cocaine. On the increase is the use of substances known collectively as “club drugs.” These are used at all-night dance parties, such as “raves” or “trances,” dance clubs, and bars. Examples are MDMA (Ecstasy), GHB, Rohypnol, Ketamine, methamphetamine, and LSD.
The safest use of drugs is no use of drugs!
Cocaine

This drug is also called blow, crack, crank, “C”, coke, nose candy, rock, and white girl.
Dangers of Use
Increases pulse rate and blood pressure. Causes insomnia, irritability, and paranoia. Can result in severe depression, convulsions, heart attack, lung damage, hallucinations, brain damage, risk of infection (hepatitis, HIV from using contaminated needles), coma, and death.
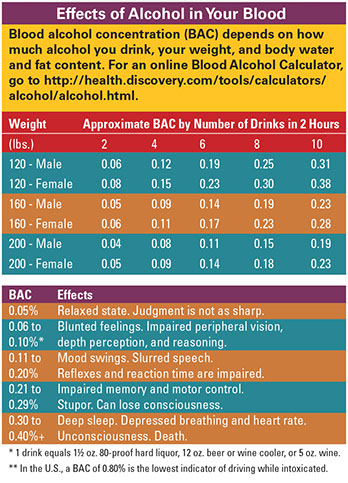
Depressants

Examples are alcohol, barbiturates, sedatives, tranquilizers, downers, ludes, reds, and yellow jackets.
Dangers of Use
Causes drowsiness, slurred speech, drunkenness, memory loss, sudden mood shifts, depression, and lack of coordination. Can result in shallow breathing, dilated pupils, clammy skin, weak pulse, coma, and death.
Ecstasy

This is MDMA. Other names are Adam, Clarity, Lover’s Speed, and K.
Dangers of Use
Euphoric state initially, but depression can occur after taking the drug. Also carries the risk of a heat stroke from lack of fluids and sweating from dancing too long, especially in the hot environment of a club. May lead to a heart attack, seizure, and stroke.
GHB and GLB
GLB is a similar drug that turns into GHB in the body. Other names are: Grievous Bodily Harm; Liquid Ecstasy, Liquid Sex, Georgia Home Boy, and Scoop.

Dangers of Use
Common date rape drug that results in nausea, vomiting, a feeling of intoxication, and amnesia-like symptoms. The drug slows the heartbeat, reduces blood pressure, and can cause the user’s breathing to stop. Overdose results in unconsciousness, coma, and eventual death. There is little difference in the dose that can get someone high and one that can cause death.
Inhalants

Examples are vapors from: Solvents, such as gasoline; aerosols, such as hair sprays; anesthetics, such as ether, chloroform, nitrous oxide; and spray paints, especially gold and silver.
Dangers of Use
Slows heart rate, breathing and brain activity. Can cause headaches, dizziness, nausea, lack of coordination, slurred speech, blurred vision. Can result in suffocation, heart failure, unconsciousness, seizures, brain damage, and even death.
Ketamine
This drug is also called: Special K, K, Vitamin K, and Cat Valium.

Dangers of Use
Causes dream-like states and hallucinations. Can cause delirium, amnesia, impaired motor functions, high blood pressure, depression, and breathing problems that can result in death.
LSD

This is also called acid, bloomers, and yellow sunshines.
Dangers of Use
Causes hallucinations, dilated pupils, increased heart rate and blood pressure, sweating, sleeplessness, dry mouth, and tremors. Nausea, weakness, numbness or trembling are common. Long term use can cause persistent psychosis and what used to be called “flashbacks” – re-experiencing symptoms of past hallucinogen use even though not taking the drug at the present time.
Marijuana

This is also called pot, grass, reefer, herb, jay, joint, smoke, weed, and AMP (marijuana with formaldehyde).
Dangers of Use
Can result in feelings of panic, impaired short term memory, decreased ability to concentrate, fatigue, paranoia, and possible psychosis. Also causes lung damage. Synthetic marijuana, such as K2 can have serious side effects, such as extremely high blood pressure, very fast heartbeat, paranoia, delusions, seizure, and hallucinations.
Methamphetamine
This drug is also called speed, ice, chalk, crystal meth, crack, fire, and glass.

Dangers of Use
Can result in memory loss, agitation, aggression, and violent or psychotic behavior and potential cardiac and neurological damage. Can contribute to higher rates of transmission of hepatitis and HIV, if injected. Can result in heart attacks, seizures, and death from overdose.
Rohypnol
This is also called R-2, Rib, Roofies, Rope, and Forget-Me Pill.

Dangers of Use
Common date rape drug. Used in sexual assaults. Results in decreased blood pressure, drowsiness, visual disturbances, confusion, nausea, and vomiting. When mixed with alcohol or other drugs, this clear, odorless, and tasteless drug can cause death.
Signs of a Drug Overdose
Signs of an overdose depend on the type of drug used. Call 9-1-1 or get emergency care for one or more of the following:
* Unconsciousness. This means the person is hard to rouse and can’t be made aware of his or her surroundings. This can be brief, such as with fainting or blacking out. It can put a person into a coma.
* No breathing or slow and shallow breathing. This means 10 or fewer breaths per minute or time lapses of more than 8 seconds between breaths.
* Slow pulse rate (40 or fewer beats per minute).
* Suicidal gestures.
* Seizures.
* Tremors.
* Sudden hostile personality or violent behavior.
* Very rapid pulse rate (140 or more beats per minute) and/or extreme anxiety or paranoia.
Resources
Alcoholics Anonymous (AA) World Services
Gives names and phone numbers for local AA groups. Gives materials on the AA program.
Al-Anon/Alateen World Service Office
A self-help program for families and friends of alcoholics. Also a referral line.
888.4AL-ANON (425.2666)
American Council for Drug Education
A substance abuse prevention and education agency for youth, college students, parents, employers, educators, and health professionals.
800.488.DRUG (488.3784)
Cocaine Anonymous (CA) World Services
Gives names and numbers for local self-help meetings.
310.559.5833
Narcotics Anonymous (NA) World Services Inc.
Gives names and phone numbers for local self-help meetings and mails out literature on narcotics to hospitals and individuals.
818.773.9999
Substance Abuse and Mental Health Services Administration (SAMHSA)
Provides a free treatment referral service to link people with community-based substance abuse services they need.
800.662.HELP (662.4357)