Women’s Health

Depression is a state of sadness and despair. Like diabetes, depression is a real medical illness. A person with depression may seek help for other problems, such as insomnia or extreme fatigue.
Signs & Symptoms
* Feeling sad, hopeless, helpless, and/or worthless.
* Fatigue. Loss of interest in life.
* Having a hard time concentrating or making decisions.
* Changes in eating and sleeping patterns.
* Feeling easily annoyed, angry, or anxious.
* Thoughts of suicide or death.
The number of symptoms and how severe they are vary from person to person.
Causes
Most likely, depression is caused by a mix of: A family history of the illness; brain chemical problems; emotional issues; and other factors, such as a medical illness or alcohol abuse.
Another cause is seasonal affective disorder (SAD). With this, depression occurs between late fall and early spring due to a lack of natural sunlight.
In some persons, extreme stress, trauma, grief, etc. may bring on depression. In others, depression occurs even when life is going well.
In general, depression is noted twice as often in women than in men in part due to hormonal changes women undergo:
* Premenstrually, during menopause, or when taking medicines with hormones.
* During and especially after childbirth or when a woman stops breastfeeding.
* After having a miscarriage.
* With health conditions that affect a woman’s hormones, such as some ovarian cysts, endometriosis, etc.
Other life circumstances unique to women may increase risk of depression, such as cultural stressors and higher rates of sexual or physical abuse.
Treatment
Whatever the cause, depression can be treated. Treatment includes medication(s), counseling, and self-care measures. Exposure to bright lights similar to sunlight can treat depression caused by SAD.
A doctor should be seen for diagnosis and treatment.
Questions to Ask
Self-Care / Prevention
* Take medications as prescribed. Get your doctor’s advice before you take over-the-counter herbs, like St. John’s Wort, especially if you take other medications.
* Don’t use illegal drugs. Limit alcohol. These can cause or worsen depression. Drugs and alcohol can also make medicines for depression less effective. Harmful side effects can happen when alcohol and/or drugs are mixed with medicine.
* Eat healthy foods. Eat at regular times. Don’t skip meals or binge on junk food. Limit caffeine and sugary foods.
* Try not to isolate yourself. Be with people you feel safe with even though you feel down.
* Do something you enjoy. Do things that let you express yourself. Write, paint, etc.
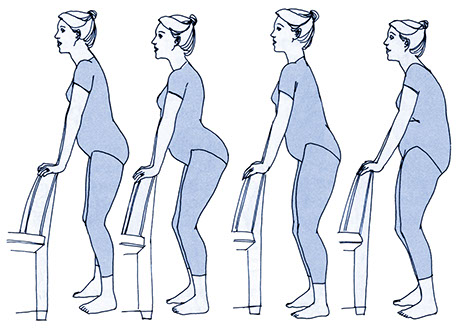
* Exercise regularly.
* Relax. Listen to soft music, take a warm bath or shower. Do relaxation exercises. Meditation can help you deal with depression.
* Keep an emergency number handy (e.g., crisis hotline, trusted friend’s number, etc.) in case you feel desperate.
Resources
Mental Health America (MHA)
800.969.6642