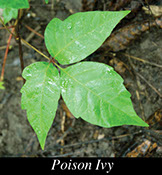
Poison ivy, oak, and sumac are the most common plants that cause a skin rash. A sap that comes from these plants causes the rash. The sap is not really a poison, but can cause an allergic reaction in some people.
Signs & Symptoms
The skin rash comes a day or two after contact with the plant. Symptoms that follow can range from mild to severe.
* Itching.
* Redness.
* Burning feeling.
* Swelling.
* Blisters.
Causes
You can get poison ivy, oak, or sumac when you touch one of these plants or touch pets, clothes, shoes, etc. that have the sap on them. Contact with the smoke of these burning plants can also cause a rash.
Treatment
Self-care treats most cases of poison ivy, oak, and sumac. For severe cases, your doctor may prescribe medicine(s).
Questions to Ask
Self-Care / Prevention
To Prevent Getting a Rash
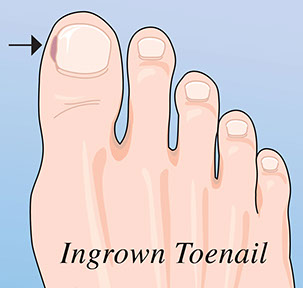
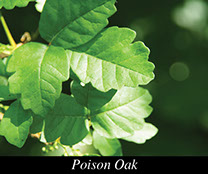
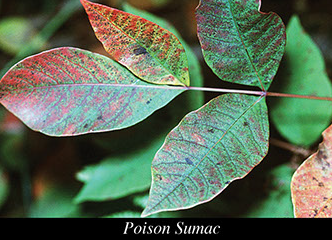
* Know what these plants look like and avoid them.
– Poison ivy and poison oak both have 3 leaflets per stem. This is why you may have heard the saying, “Leaflets three, let them be.”
– Each branch of poison sumac has 7 to 13 leaflets on a reddish stem. A single leaf is on the end of the stem. The others are paired along each side of the stem. Poison sumac grows in wetlands.
* Use an over-the-counter lotion (IvyBlock), which blocks skin contact with the sap. Use it as directed.
* Wear pants and long-sleeved shirts.
* Use an over-the-counter product (e.g., Tecnu) that removes poison ivy sap.
* Rinse the affected area with water.
* To help prevent an allergic reaction, do the things listed below. Do them within 6 hours of contact with one of the plants.
– Remove all clothes and shoes that have touched the plant.
– Wash the skin area well with soap and water.
– Use an over-the-counter product (e.g., Tecnu) that removes poison ivy sap.
To Treat Poison Ivy, Oak, or Sumac
* Take a cold shower, put the rash area in cold water, or pour cold water over it. Use soap when you shower.
* To relieve itching, take an over-the-counter antihistamine, such as Benadryl. Follow the label’s directions.
* For weeping blisters, mix 2 teaspoons of baking soda in 4 cups of water. Dip squares of gauze in this mixture. Cover the blisters with wet gauze for 10 minutes, 4 times a day. Do not apply this to the eyes.
* Wash all clothes and shoes with hot water and a strong soap. Bathe pets that have come in contact with the plant. The sap can stay on pets for many days. Clean items used to wash clothing and pets. Wear rubber gloves when you do all these things.
* Keep your hands away from your eyes, mouth, and face.
* Do not scratch or rub the rash.
* Take baths with lukewarm water. Add an over- the-counter product called Aveeno colloidal oatmeal.
* Apply any of these to the skin rash:
– Calamine (not Caladryl) lotion.
– Over-the-counter hydrocortisone cream. Follow the directions on the label.
– A paste of 3 teaspoons of baking soda and 1 teaspoon of water.