Abdominal & Urinary Conditions
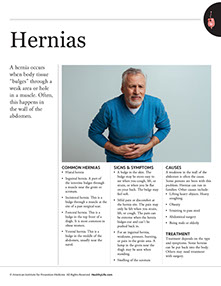
A hernia occurs when body tissue “bulges” through a weak area or hole in a muscle. Often, this happens in the wall of the abdomen.
Signs & Symptoms
* A bulge in the skin. The bulge may be more easy to see when you cough, lift, or strain, or when you lie flat on your back. The bulge may feel soft.
* Mild pain or discomfort at the hernia site. The pain may only be felt when you strain, lift, or cough. The pain can be extreme when the hernia bulges out and can’t be pushed back in.
* For an inguinal hernia, weakness, pressure, burning, or pain in the groin area. A lump in the groin near the thigh may be seen when standing.
* Swelling of the scrotum.
Causes
A weakness in the wall of the abdomen is often the cause. Some persons are born with this problem. Hernias can run in families. Other causes include:
* Lifting heavy objects. Heavy coughing.
* Obesity.
* Straining to pass stool.
* Abdominal surgery.
* Being male or elderly.
Treatment
Treatment depends on the type and symptoms. Some hernias can be put back into the body. Others may need treatment with surgery.
Questions to Ask
Self-Care / Prevention
* Don’t smoke. If you smoke, quit. Avoid secondhand smoke.
* Maintain a healthy diet. Lose weight if you are overweight.
* Avoid constipation. Don’t strain to pass stool.
* Exercise to keep abdominal muscles strong. Follow your doctor’s advice.
* When you do sit ups, keep your knees bent and your feet flat on the floor.
* Follow proper lifting techniques.
* Wear a weight lifting belt to support the back when lifting.
* Wear a truss. This is a device that holds a hernia in place.
* For mild pain, take an over-the-counter medicine for pain. If even mild pain lasts longer than a week, see your doctor.
Common Hernias Include
* Hiatal hernia.
* Inguinal hernia. A part of the intestine bulges through a muscle near the groin or scrotum.
* Incisional hernia. This is a bulge through a muscle at the site of a past surgical scar.
* Femoral hernia. This is a bulge in the top front of a thigh. It is most common in obese women.
* Ventral hernia. This is a bulge in the middle of the abdomen, usually near the navel.