The Heimlich maneuver can be used to clear an object blocking the airway in conscious adults and children ages 1 to 8. It lifts the diaphragm and forces air from the lungs to push the object that blocks the airway up and out.
Persons Over 8 Years Old
1. Ask, “Are you choking?”
The person may use the choking sign. Do not interfere if he or she can speak, cough, or breathe.
2. If not able to speak, cough, or breathe, reach around the person’s waist from behind.
Make a fist. Place it above the navel, but below the rib cage. Grasp your fist with your other hand. Press your fist into person’s abdomen and give 5 quick, upward thrusts. See image A.
3. Repeat upward thrusts until the object is forced out or the person becomes unconscious.
If the object is removed with success, the person should see a doctor as soon as possible.
4. If the person becomes unconscious, shout for help! Call 9-1-1!
Tilt the head back and lift the chin to open and check the airway. {Note: If you suspect the person has a head, neck, or spine injury, do not move him or her. Pull the lower jaw forward to open the airway.} Give 2 slow rescue breaths. If this doesn’t help, tilt the head further back (if no head, neck, or spine injury). Give 2 rescue breaths again. If the person does not respond or move, give 30 chest compressions. See image B. Repeat rescue breaths and chest compressions. Each time you open the airway to give rescue breaths, check the person’s mouth for the object and remove it if you can. Do CPR as needed, until the object blocking the airway is forced out or until medical help takes over.
5. Even when the object is removed with success, the person should see a doctor as soon as possible.
Children Ages 1 to 8
1. For a conscious child, give abdominal thrusts as for adults. Don’t be too forceful.
2. For an unconscious child, give first aid for choking as for an adult.
Babies Up to 1 Year Old
1. Do not interfere if the baby coughs strongly, cries, or breathes okay.
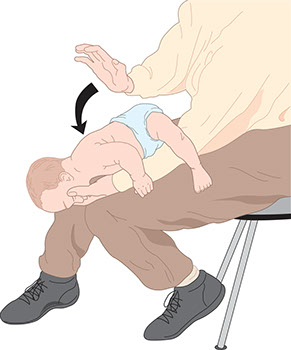
2. If the baby is conscious, hold the baby’s head (face down) in one hand. Straddle the baby over your forearm. Rest your forearm on your leg for support. Keep the baby’s head lower than the rest of his or her body.
3. With the heel of your free hand, give up to 5 quick, forceful blows on the baby’s back between the shoulder blades. See image C. If the object still blocks the airway, go to step 4.
4. Turn the baby over (face up). Cradle the baby on your forearm. Support the head with one hand. Keep the baby’s head lower than the rest of his or her body. Rest your arm on your leg for support. Place 2 fingers 1/2 inch below and in between the nipples on the baby’s chest. Give 5 quick downward thrusts. Depress the sternum about 1-1/2 inches with each thrust.
5. Repeat steps 3 and 4 until the object is removed or the baby is unconscious.
6. If the baby is unconscious, shout for help. Have someone call 9-1-1! If no one calls 9-1-1, give first aid for 1 minute, stop to call 9-1-1, then resume rescue efforts.
7. Put the baby on his/her back. Keep the head tilted back with one hand and give 30 chest compressions using 2 fingers on your other hand. Give 2 slow rescue breaths. If the object is expelled, stop. If not, give cycles of 30 compressions and 2 slow rescue breaths until the object is removed or help arrives.
8. Check for and remove the object in the airway, if visible. Repeat steps 7 and 8 as needed.
9. Don’t give up! Give CPR until medical help takes over or until the object is removed. Even if it is, get medical care right away.