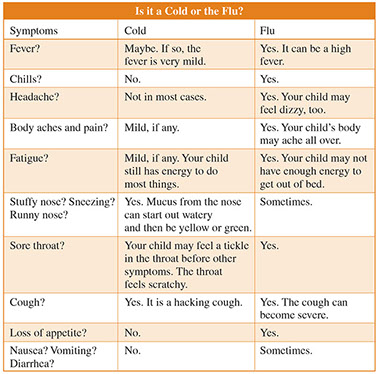
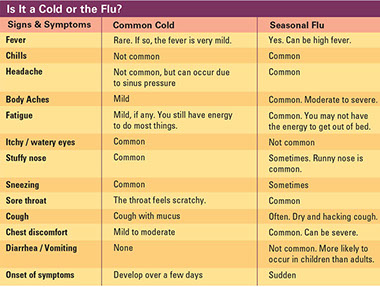
Cold symptoms mostly affect you above the neck. Flu symptoms affect the body all over. Signs and symptoms for colds and flu vary from person to person. On average, adults get about 1 to 3 colds a year. Children get about 6 colds a year.
Signs & Symptoms
More Information
Colds and flu are very contagious.
Cold symptoms usually appear 2 or 3 days after you pick up a cold virus. A cold can last from 2 to 14 days. Most people recover in a week. The cough that comes with a cold can last a few weeks after other symptoms go away. If you get cold symptoms often or they last much longer than 2 weeks, you might have an allergy, not a cold.
People infected with the flu may be able to infect others from 1 day before they get sick to 5 to 7 days after getting sick. Children and people with weakened immune systems could be contagious for more than 7 days.
Causes & Risk Factors
Colds and flu are caused by viruses. These spread:
* Through breathing air droplets made when an infected person coughs, sneezes, or talks.
* By touching an object with the virus on it and then touching your nose, mouth or eyes.
Common Cold
The common cold is caused by more than 200 viruses. This is one reason why there is no cure for the common cold.
Flu
Flu is short for influenza. There are many kinds of flu. These include:
* Seasonal flu. This flu comes every year during fall and winter, but can last through May. Each year, different strains of type A and/or type B viruses cause this kind of flu. Scientists try to match the viruses in the flu vaccine to those that are most likely to cause flu for that flu season.
* H1N1 flu. This is caused by H1N1 virus. It was first detected in people in Mexico and the U.S. in April of 2009. It used to be called swine flu.
* Pandemic flu. This is any type of flu that causes a global outbreak of serious illness that spreads easily from person to person. H1N1 flu was declared a pandemic in June of 2009.
* Bird (avian) flu. This is caused by avian influenza A (H5N1) virus which normally infects wild birds. Contact with infected birds or surfaces they contaminate can spread this virus to humans. The viruses may be able to change to a form that could spread from person to person and result in a widespread infection in humans.
Prevention
Wash your hands often with soap and water. Take at least 20 seconds each time.
When you can’t wash your hands, use alcohol-based wipes or gels to clean your hands. Rub the gel form into your hands until they are dry.
* Avoid touching your eyes, nose, and mouth.
* Cover your nose and mouth with a tissue when you cough or sneeze. Throw the tissue away. If you do not have a tissue, cough or sneeze into your elbow or upper sleeve.
* Try to avoid close contact with people and their things when they have a cold or flu symptoms.
* Keep your distance from others if you are sick.
* When possible, stay home from work, school, and errands when you are sick. Don’t send your children to childcare or school if they are sick.
* Clean and disinfect commonly used objects and surfaces. Examples are doorknobs, phones, railings, light switches, and remote controls.
Good Times to Wash Your Hands
* After you cough, sneeze, or blow your nose
* Before you touch your eyes, nose, and mouth
* After using the bathroom
* After shaking hands
* After you touch door handles, phones, and other objects and surfaces that others touch or cough or sneeze on
* Before you eat and/or prepare food
* When you come into contact with someone who is sick
* Follow your doctor’s advice for vaccines, antiviral medicines, and other ways to help protect you from the flu.
* Stay healthy to fight off infections:
– Eat nutritious foods.
– Do regular exercise.
– Manage stress.
– Get enough sleep.
* The single best way to protect against getting the flu is to get a yearly vaccine for seasonal flu.* All persons aged 6 months and older should get a flu vaccine. It comes in two forms:
– A flu shot. Note: Consult your health care provider if you have had a severe reaction to the vaccine in the past or have a severe allergy to eggs or any part of the vaccine.
– A nasal spray. This is approved for people aged 2 to 49 years. Pregnant women should not get this form.
{*Get up-to-date advice for vaccines at 800.CDC.INFO (232.4636) orwww.cdc.gov/vaccines.}
Medical Care
Antibiotics do not treat cold and flu viruses. Antibiotics treat infections from bacteria.
* Taking antibiotics for viruses is the main cause of antibiotic resistance. With this, bacteria that were once fought off by antibiotics have become stronger than the medicine.
* Certain bacteria have become so resistant that it is hard to find an antibiotic that is able to treat the infection. An example is Methicillin-resistant Staphylococcus aureus (MRSA). This can cause an infection that affects the skin or causes pneumonia. MRSA resists treatment with usual antibiotics.
* If you get the flu, call your doctor’s office. Describe symptoms. Ask if flu testing, an antiviral medicine, or medical care is needed.
* Prescribed antiviral medications can make flu symptoms milder and help you get better sooner if started:
– Within 48 hours of the start of symptoms for adults
– Within 36 hours of the start of symptoms for children
Get up-to-date information on treatment for different kinds of flu from The Centers for Disease Control and Prevention (CDC) at 800.CDC.INFO (232.4636) orwww.cdc.gov/flu.
Reasons to Contact a Doctor
* You wheeze or have trouble breathing.
* A baby less than 3 months old has a fever between 99.5°F and up to 100.4°F.
* A person age 3 to 65 years old has a fever over 104°F.
* A person age 65 years and older has a fever of 102°F or higher.
* A child between 3 months and 3 years old has a fever of 102.2°F or higher.
* A bad smell comes from the throat, nose, or ears.
* An earache persists.
* A sore throat is bright red or has white spots.
* Pain or swelling over the sinuses worsens with bending over or moving the head, especially if you also have a fever.
* Yellow or green sputum or nasal discharge lasts longer than 5 days.
* Flu symptoms last longer than a week and self-care brings no relief.
* Cold symptoms get worse after 4 to 5 days or don’t get better after 7 days.
* Symptoms other than a slight cough last for more than 14 days.
Reasons to Get Medical Care Fast
* Breathing is very fast (over 40 breaths per minute).
* Extreme shortness of breath or trouble breathing
* The skin, lips, or fingernails have a bluish color.
* Severe wheezing or a severe cough
* A baby less than 3 months old has a fever of 100.4°F or higher. A child 3 months to 3 years old has a fever of 104°F or higher.
* Not waking up or not responding
* Coughing up true, red blood
* Pain or pressure in the chest or abdomen
* Severe or persistent vomiting
* Sudden dizziness. Confusion.
* A red or purple rash does not fade when pressure is applied to the skin.
* Stiff neck; seizure; or a severe headache that persists
* A child is so irritable that he or she does not want to be held.
* Flu symptoms improve, but return with a fever and a worse cough.
Self-Care
Self-care measures treat most cases of colds and flu. People with chronic health problems should consult their doctors or health care providers for advice to manage symptoms.
* Rest and drink lots of liquids.
* Take an over-the-counter (OTC) medicine to lower fever and relieve pain, if needed. {Do not give aspirin to anyone under 19 years old. Aspirin and other medicines with salicylates have been linked to Reye’s syndrome.}
* Use a cool-mist vaporizer to add moisture to the air.
* For nasal congestion, use salt water drops or a saline nasal spray.
* Have chicken soup to help clear mucus.
* Gargle every few hours with warm salt water. (Dissolve ¼ teaspoon of salt with 1 cup of warm water.)
* Suck on a piece of hard candy or medicated lozenge. Note: Do not give these to children younger than 5 years old.
* If you use OTC medicines for cold and cough symptom relief, be careful. Read the warnings on the label. Ask your doctor or pharmacist which products are safe for you to use. Note: Do not give OTC cold and cough medicines to children under 6 years old. For children 6 years old and older, follow their doctor’s advice.
* To soothe a sore throat, have warm drinks, such as tea with lemon and/or honey. Note: Do not give honey to a child under 1 year old due to the risk of botulism.
* Check with your doctor or health care provider about using zinc lozenges, echinacea, and/or vitamin C when cold symptoms start.
* To avoid spreading cold and flu viruses, follow tips in “Prevention.”
Respiratory Syncytial Virus (RSV)
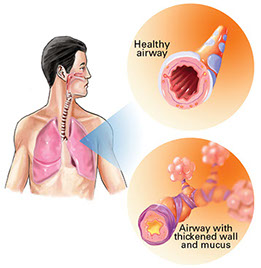
Respiratory Syncytial Virus (RSV) is an infection of the lungs and breathing tubes.
* In adults and children over 3 years old, symptoms are like those of a cold.
* In children under 3 years old, RSV can cause a lower respiratory infection, such as pneumonia. Infants 2 to 6 months old are more prone to this.
Get medical care right away if your baby has signs and symptoms of RSV:
* Blue color around the lips, fingernails, or skin
* Quick breathing or trouble breathing
* Grunting sounds with breathing
* Fever of 100.4ºF or higher in a baby less than 3 months old; 104ºF or higher in a child between 3 months and 3 years old.
* Severe cough or severe wheezing
Resources
Centers for Disease Control and Prevention (CDC)
800.CDC.INFO (232.4636)
www.flu.gov
www.cdc.gov/flu