Back pain can be sharp, dull, acute, or chronic. It can be felt on one or both sides of the back.
Causes
Low Back Problems
Back pain occurs most often in the lower back. That is where the human body absorbs the most weight and stress. About half of working age adults have low back problems. Having an acute low back problem means lower back or back-related leg symptoms for less than 3 months. About 90 percent of persons with acute low back problems resume normal activity within a month with or without medical treatment. Often, acute low back pain goes away on its own in a few days or weeks.
Sprains and Strains
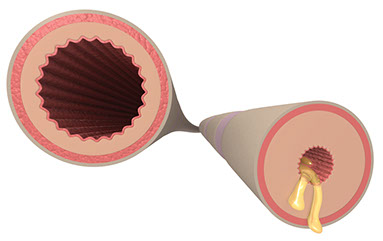
A sprain is an injury to a ligament (fibrous tissue that connects bones). A strain is an injury to a muscle or tendon (tissue that connects muscle to bone). Most backaches come from strained muscles in the lower back or from sprained ligaments that support the spine.
Poor Posture
People who slouch put strain on their backs. Poor posture can cause back pain and limit recovery efforts. The back has three natural curves: one at the neck, one at the middle back, and one at the lower back. A healthy spine and flexible muscles support the spine and keep the body in proper alignment. With good posture, all three curves are balanced and the ears, shoulders, and hips are aligned.
Lack of Exercise
Muscles that aren’t worked out regularly are more prone to injury. Do whole body exercises, such as swimming and/or walking. Do exercises that stretch and strengthen your back, too.
Excess Weight
Ten extra pounds of body weight puts 30 pounds of strain on the lower back. Being very overweight increases the weight on the spine, putting increased pressure on the discs in the spine. The discs allow the vertebrae to move more smoothly.
Stress
Stress can worsen back pain that already exists. Back spasms may even be caused by worries and fatigue. These exercises can help reduce stress:
* Sit comfortably. Breathe deeply. Tighten and relax each muscle of your body from head to toe. Hold each muscle tight for five seconds and then relax.
* Picture relaxing scenes and go there in your mind.
Other Causes of Back Pain
* Arthritis
* Back injury, such as from a fall or an accident
* Fibromyalgia
* Kidney stones
* Infections (bladder, kidney, lung, etc.)
* Osteoporosis
* Ruptured disc or other mechnical problem in the spine
* Sciatica. This is inflammation of the sciatic nerve. This nerve starts in the lower spine and goes down the back of the legs.
Prevention
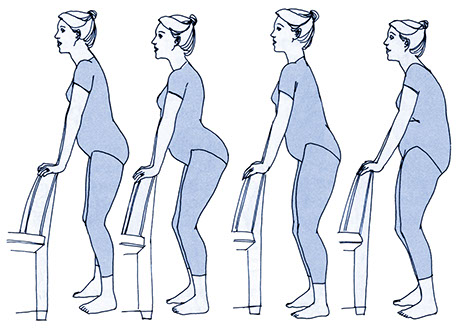
When You Lift Things
Do’s
* Wear good shoes (not sandals) with low heels.
* Stand close to the object.
* Plant your feet squarely, shoulder width apart.
* Bend at the knees, not at the waist. As you lift, slowly straighten your knees.
* Hold the object close to your body.
* Lift slowly. Let your legs carry the weight.
* Get help or use a dolly to move something that is too big or very heavy.
Don’ts
* Don’t lift an item that is too heavy. Get help or use a mechanical lifting device.
* Don’t lift anything heavy if you’re not steady on your feet.
* Don’t bend at the waist to pick something up.
* Don’t arch your back when you lift or carry.
* Don’t lift too fast or with a jerk.
* Don’t twist your back when you are holding something. Turn your whole body, from head to toe.
* Don’t lift something heavy with one hand and something light with the other.
* Don’t try to lift one thing while you hold something else. For example, don’t pick up a child while you are holding a grocery bag. Put the bag down and lift the bag and the child together.
When You Reach for Things
Do’s
* Get close to the object you are reaching for.
* Use a sturdy step stool or a ladder to reach higher than your shoulders. Or use a tool made for reaching things.
* Tighten your stomach muscles.
* Let your arms and legs do the work.
* Turn your whole body to move the object.
Don’ts
* Don’t stretch your back or overstretch your arms to reach an object.
* Don’t twist your upper body.
When You Sit
Do’s
* Sit on chairs that are low enough so both of your feet are flat on the floor or use a footrest. Keep your knees level with your hips.
* Sit against the back of the chair.
* Use a lumbar support or rolled towel for lower back support.
* Take frequent mini-breaks to walk, stretch, and change your activity.
Don’ts
* Don’t slouch.
* Don’t lean forward and arch your back in a chair that’s too high or too far from your desk.
When You Sleep
Do’s
* Sleep on a firm mattress or surface.
* Get comfortable when you lie down or sleep.
* If you sleep on your back, keep your upper back flat, but your hips and knees bent. Keep your feet flat on the bed. Tip your hips down until you find the best spot. Put a pillow under your knees if that feels good to you.
* If you sleep on your side, keep your knees bent. Put a pillow between your knees.
* When you get up from bed, move slowly, roll on your side and swing your legs to the floor. Push off the bed with your arms.
Don’ts
* Avoid soft, sagging mattresses.
* Don’t sleep on your stomach.
When You Walk or Stand
Do’s
* When standing for long periods, prop one foot up.
* Shift your weight from one foot to the other.
* When standing and walking, keep all 3 curves of the back balanced and the ears, shoulders, and hips aligned.
* Wear low-heeled, comfortable shoes.
* Use proper posture. (Head high, chin tucked, and toes straight ahead.)
Don’ts
* Don’t stay in one position too long.
* Don’t bend forward when your legs are straight.
* Don’t walk with poor posture.
* Avoid high-heeled or platform shoes.
When You Drive
Do’s
* Keep your knees level with your hips. Adjust the car seat forward, if you need to.
* Sit up straight and keep both hands on the wheel.
* Use a lumbar support or rolled towel for lower back support.
Don’ts
* Don’t sit too far from the wheel. Stretching for the pedals and steering wheel strains the back.
If you are overweight, lose weight.
* Get regular physical activity.
* Stretch before and after you exercise or work.
* Don’t smoke. If you smoke, quit. Smoking increases the risk of osteoporosis. It also slows the healing of damaged disks of the spine.
* Reduce emotional stress that causes muscle tension. Learn to deal with stress.
– Several times a day, do a “body check” for tensed muscles and let them relax.
– Balance work and play. Plan some “me” time.
– Do relaxation and deep breathing exercises. Do yoga, tai chi, or meditate.
– Seek professional help for stress, if needed.
Back Exercises
You can help improve a bad back, maintain a healthy back, and decrease your risk of back injury by exercising your back. Contact your doctor or health care provider before you start a new exercise program. Start slowly. Stop if pain increases.
Ask your health care provider about other back exercises. Ask, too, about an aerobic exercise program, such as walking, running, swimming, or biking.
Do back exercises for 15 minutes a day, 3 to 5 times a week.
Pelvic Tilt
This strengthens front and back muscles and helps prevent swayback. Lie on your back with knees bent. Keep your feet flat on the floor. Breathe slowly and deeply. Rest your arms at your sides. Get comfortable and relaxed. Tighten your stomach muscles so the small of your back is flat on the floor. Next, begin to tighten the buttock muscles. Tilt the hips or pelvis upward, and relax. Hold for a count of 5. Repeat 5 times.
Knee-to-Chest Raise
This limbers up a stiff back. Lie on your back with knees bent, feet flat on the floor. Breathe deeply. Get comfortable and relaxed. Raise your right knee to your chest and grasp it with both arms. Hug your knee in order to feel a slight stretching in the lower back region. Hold for a count of 5. Do this 5 times. Repeat with your left leg. Repeat with both legs. Be careful not to arch your back. Don’t use your arms to lift your legs.
This increases flexibility of the spinal column. Stand erect and raise both hands over your head. Stretch towards the ceiling. Focus on your upper body. Use your arms, hands, and fingers to reach upward as though you were being pulled upward. Keep your feet flat on the floor. Hold for a count of 5.
Curl Up
This strengthens the lower back. Lie on your back while on a firm surface. Slowly bring both knees to your chest and bring your chin forward to your chest. Your arms should be extended straight at your sides. Hold for a count of 5. Gradually return to your starting position.
Elbow Props
These strengthen low back muscles and help maintain the normal curve of the lower back. Lie on your stomach. Turn your head to one side. Relax your arms at your sides. Relax like this for 3 minutes. Prop up on your elbows with your head facing forward. Keep your lower back completely relaxed and flat. Hold this position for 2 minutes. Return to the starting position for 1 minute. Repeat 3 times.
Sitting Hamstring Stretch
This warms up and limbers the back muscles and stretches the hamstring muscles. Sitting on the floor, stretch your right leg out directly in front of you. Place your left foot under your right knee. The toes of your right leg should be pointed upward. Slowly reach forward to grasp the tips of your right toes. Be careful to bend over from the hip. Hold for a count of 10. Repeat 5 times. Then switch leg positions.
Treatment for Low Back Pain
Continue your regular activities as much as you can. Back muscles can get weak if you don’t use them. Rest your back, if you must, but don’t rest in bed for more than 1 to 2 days, even if your back hurts a lot. Bed rest should only be used for persons with severe limitations (due mostly to leg pain).
{Note: Before you seek treatment for back pain on your own, check with your doctor or health care provider. Discuss the benefits and risks for treatments, such as spinal manipulation, different forms of massage, and herbal remedies.}
Medication
* Over-the-counter (OTC) pain relievers. Examples are acetaminophen, aspirin, ibuprofen, ketoprofen, and naproxen sodium. These relieve back pain, but only for a short time. All but acetaminophen also reduce swelling and are called NSAIDs+. This stands for nonsteroidal anti-inflammatory drugs.
* Prescribed NSAIDs+ and other medicines, such as muscle relaxants.
+ NSAIDs can cause stomach upset, indigestion, and ulcers in the stomach and intestines. Discuss the benefits and risks of taking NSAIDs, as well as other medicines, with your doctor.
Cold Treatment
Injury to the back can cause blood vessels to tear. This leaves a bruise. Cold inhibits bruising and swelling and numbs pain. Cold packs, like crushed ice wrapped in a towel, can help. Apply a cold pack for 5 to 10 minutes at a time, several times a day. For best results, lie on your back with your knees bent and place the ice pack under your lower back. Start right after a back strain. Do this for 10 minutes every 2 hours for the first 48 hours.
Heat Treatment
Unlike cold, heat increases blood flow to the affected area. This promotes healing. Wait at least 48 hours after back symptoms start to apply heat. If heat is used sooner, the increased blood flow can add to the swelling. Heat can be applied with moist heating pads, hot-water bottles, hot compresses, hot tubs, and hot baths or showers. Use heat for 10 minutes at a time. Do this several times a day.
Massage
Massage won’t cure a backache. It can increase blood flow to tight muscles and loosen them.
Braces or Corsets
Braces and corsets support the back and keep you from moving it too much. They won’t make your back stronger, though.
Medical Care
Reasons to Get Immediate Medical Care
* Back pain spreads to the chest, neck, arm, or lower jaw.
* The pain started in the chest and moved to the upper back.
* The pain follows a fall or impact injury to the back.
* Back pain occurs with passing out, lightheadedness, or difficulty with balance or coordination.
* You can’t move due to the pain or it is hard to move an arm or a leg after a fall or back injury.
* A new loss of bowel or bladder control occurs with back pain.
* Back pain occurs with severe abdominal or pelvic pain.
* A “tearing” type of pain is felt in the back or a pulsating mass is felt in the abdomen.
* Loss of sensation is felt in the rectal area.
Reasons to Contact a Doctor
* Severe back pain occurs for more than 7 days or the pain travels down a leg below a knee.
* Weakness, numbness, or tingling in the feet or toes occurs with back pain.
* Back pain occurs with: Pain, burning, or itching when you urinate; increased urge to urinate; urinating often; foul-smelling urine; or blood in the urine.
* An unusual discharge from the vagina or urethra occurs with back pain.
* A sharp pain is felt in a buttock and may spread to the thigh, knee, or foot.
* Back pain occurs with: A fever; nausea or vomiting; a skin rash; or mild to moderate abdominal or pelvic pain.
* Pain increases with moving, coughing, lifting, or straining.
Resources
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
877.22.NIAMS (226.4267)
www.niams.nih.gov