There are two ways a baby may be born:
* Through the vagina (vaginal birth). Contractions of the uterus push the baby out through the cervix into the vagina. The baby passes through the vagina to enter the world.
* Cesarean section (C-section). This is a surgical method. The baby is taken directly from the uterus.
The type of delivery you have will depend on your needs. Discuss the options with your health care provider.
Vaginal Births
Natural childbirth means that no medication is given to induce (bring on) labor. Little or no medicine is given to relieve pain. The mother uses various methods to aid the delivery process, like special breathing. Her “coach” provides support.
Vaginal births can also involve medicines. Some of these are:
* Misoprostal. This tablet is put in through the vagina to help dilate the cervix.
* Pitocin. This is a hormone that causes the uterus to contract. It helps to start or speed up labor. It is given through an IV (intravenous drip).
* Prostaglandin gel. This is a gel that is put in through the vagina. It goes right on the cervix. It can help dilate the cervix. It also causes the uterus to contract. This helps to start labor.
* Narcotic pain relievers. Example: Demerol. These can be given with a shot or an IV. They take the edge off pain. But they can also cause you to feel drowsy or dizzy. They can cause an upset stomach or throwing up. Other medicines may be given with narcotic pain relievers. These help them have a stronger effect.
* Tranquilizers. These relax you if you are tense and anxious. They can be given in pills or with a shot. Tranquilizers are sometimes used with pain relievers.
* Anesthetics. Anesthetics cause a loss of feeling. They are usually given after labor has been in progress. There are two main types:
* General anesthesia. This puts the mother to sleep. It is used most often for emergency C-sections. But it can be used in a vaginal birth when the baby is in a breech position. That’s when the baby’s bottom or one or both feet reach the cervix before the head does.
* Local anesthetics. These affect only the area where they are applied. Common examples:
– Pudendal block. A shot numbs the nerves in the vaginal area. It is usually given when the cervix is fully dilated (opened). It may be used with a pain reliever or tranquilizer.
– Epidural block. This is the most popular anesthetic used for labor. The mother lies on her left side or she sits up and leans forward. A shot is given in the back to numb the area. A thin plastic tube is put into the epidural space of the spine. Medicine is given through the tube. This causes some loss of feeling from the waist down. How much numbness occurs depends on the drug and dose used. An epidural block can have other effects. It can lower the mother’s blood pressure. It can make her unable to pass urine on her own. In that case, a tube called a Foley catheter is used to empty urine from the bladder. An epidural block can also increase the chance that forceps will be used at delivery. {Note: Just pain medicine can be given through the tube. It does not cause a loss of feeling from the waist down. If this is done, the mother may be able to get out of bed and walk. But an adult should be with her.}
Whether or not pain medicine is used is not what matters most. The goal in labor and delivery is to have a healthy baby and a healthy mother.
Cesarean Births
A C-section requires anesthetics. Either an epidural block or spinal is used. General anesthesia is rarely used. C-sections are usually done with a low, left-to-right incision (cut) near the line of pubic hair. This is called a lower-segment incision or a “bikini” cut. An up-and-down incision is rare these days. But it may be used in an emergency. The type of incision in the skin may be different from the one made in the uterus.
C-sections may or may not be planned. Here are some reasons for doing one:
* The baby (or babies) or mother is not doing well
* The baby is too big for the mother’s pelvis
* The mother has placenta previa or placenta abruptio.
* The mother had a past C-section with an up-and-down incision on the uterus.
* The baby is lying in a way that makes it hard to deliver.
* The mother has an active outbreak of genital herpes.
* Labor does not progress the way it should.
* The umbilical cord is wedged between the cervix and the baby. This cuts off blood flow to the baby.
* The mother is not strong enough for a vaginal delivery.
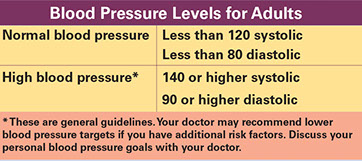
* The mother has health problems, like diabetes, high blood pressure, kidney disease, or preeclampsia.
* The baby is more than 2 weeks late and the placenta does not nourish the baby well.
Vaginal Births after C-Section (VBAC)
Some pregnant women have already had a C-section delivery. Of this group, some might be able to have a safe vaginal delivery. Some might not for the next baby.
A vaginal delivery after a C-section may be possible if:
* The incision for the C-section was the left-to-right, lower-segment type.
* Your pelvis is normal size.
* Reasons for the past C-section are not present now. Examples:
– Breech baby
– Separation of the placenta (placenta abruptio)
– More than one baby
– Baby in distress
Signs of Prelabor
Prelabor is the period just before labor begins. Call your health care provider if any of these signs of prelabor happen more than one month before your due date:
* The baby begins to settle into your pelvis. It looks and feels as if the baby has “dropped.” This process is called lightening and engagement. It’s easier for you to breathe after it happens.
* You feel more pressure on the pelvis and rectum (rear end). The pressure can cause a dull ache in the pelvic area or lower back. It feels like menstrual cramps.
* Vaginal discharge may increase and thicken.
* Your energy level changes. Some women feel less energy. Others feel more. They want to clean the whole house. The “nesting instinct” is a way of getting ready for the new baby.
* You lose the mucus plug. That’s a blob of thick stuff that blocks the cervix. You can lose it several days before labor starts. Or you can lose it just as labor starts.
* You may see the bloody show. When the cervix opens, small blood vessels often break. The blood colors the mucus plug pink. Or it may streak the mucus plug with red. When the mucus plug falls out, you may see the blood. You may pass a big clump that looks like a wet cotton ball. Some women don’t notice the bloody show. Bloody show usually means that labor will start within 24 hours. But sometimes labor could still be a few days away.
* You have diarrhea. Some women get this just before labor starts.
* The “bag of waters” (or your “water”) breaks. That’s the sac inside the uterus. It holds the amniotic fluid. The baby grows there. About 15 percent of the time, the water breaks before labor starts. More often, this happens during labor. The fluid can come out in a gush or a slow trickle. Call your provider right away if this happens.
1st Stage of Childbirth
The First Stage of Childbirth: Labor
Labor has three parts:
* The first part is called early or latent labor. This is usually the longest part. It’s usually the least painful, too.
– Real contractions begin. Contractions are when the muscles of the uterus tighten and then relax. The feelings usually start in the lower back and travel to the belly. Some contractions are felt only in your back. Others are felt only in your belly. Contractions usually start about 15 to 20 minutes apart and last 30 to 45 seconds.
– The cervix dilates to open 3 centimeters across. That’s about the size of a silver 50¢ piece. It gets thinner. This can happen over a period of days or weeks. You may not even be aware of it. Or it can happen with stronger contractions over a period of 2 to 6 hours. Rarely, it could take up to 24 hours with the stronger contractions.
– Call your health care provider during the first part of labor. Your provider may tell you to go to the hospital or birthing center. Make sure you’re packed!
* The second part is called active labor. This part of labor is usually shorter than the first part. On average, it lasts 2 to 3 hours. But its length can vary greatly. If you’re not already at the hospital or birthing center, you should get there early in this part of labor. Signs of this part of labor:
– Contractions are stronger. They come more often, usually every 3 to 4 minutes. They last longer, from 40 to 60 seconds each.
– The cervix dilates to 7 centimeters. That’s about the size of the rim of a coffee mug.
* The third part is called advanced active labor or transition. It is the most tiring part. But it is also the shortest. The average length is 15 to 60 minutes. Here are signs that you are in transition:
– Contractions are even stronger. They come every 2 to 3 minutes. Each lasts 60 to 90 seconds.
– The cervix dilates fully. It opens 7 to 10 centimeters. That’s about the size of a small grapefruit.
2nd Stage of Childbirth
The Second Stage of Childbirth: Delivery
During delivery, you push the baby down the birth canal and out into the world.
* Contractions continue. They are usually more regular than before. They come less than two minutes apart. Each lasts about 60 to 90 seconds. You only push when you have contractions. Your health care provider will tell you when to push.
* Most babies come out head first. Then the shoulders. After this, the rest of the baby’s body slips out with ease. Your baby may be placed on your tummy.
* The umbilical cord is clamped and cut.
* The time for this stage varies greatly. It can take from 10 minutes to 3 hours or more.
3rd Stage of Childbirth
The Third Stage of Childbirth: Delivery of the Placenta
Delivery of the placenta usually lasts from about 5 to 30 minutes. Delivery takes place through mild contractions. You might not even feel them. One more push from you can help the placenta come out. Or a nurse or your health care provider may gently press down on your abdomen. This, too, can help the placenta come out.
{Note: The total time for labor varies from woman to woman. It also varies from pregnancy to pregnancy for the same woman. First babies tend to take longer than later ones. This is not always the case, though.}
During Labor
Things Your Health Care Provider May Do During Labor
Your health care provider and his or her staff may do any of the things below during labor. What they will do depends on your special needs. But find out ahead of time which ones the provider is sure to do.
* Do a physical exam.
– Your provider feels your belly. This helps the provider know how big the baby is. It helps the provider to know how the baby is lying.
– Your provider gives you a pelvic exam. This shows how open and thin your cervix is. Your “bag of waters” could break by itself during this exam.
* Put an IV (intravenous drip) in a hand or arm vein. Here are reasons why this may be done:
– To give you fluids. This keeps you from getting dehydrated (dried out or without enough body fluids).
– To give you glucose. Glucose is a type of sugar. It gives you energy. This will help if you have a long labor.
– To provide a way to give you medicine quickly, if you need it.
* Use a fetal monitor to check the baby. This small machine can check your baby’s heartbeat before the baby is born. It can also record your contractions. There are 2 kinds of fetal monitors:
– External monitor. This kind has two wide straps. The straps go over your belly. One strap picks up your baby’s heartbeat by ultrasound. The other connects to a pressure gauge. The gauge records your contractions on a printout.
– Internal monitor. This kind has a small tube that goes inside the uterus. The “bag of waters” must be broken before this monitor can be used. It gets there through the vagina and cervix. A small electrode goes on the baby’s head. This monitor gives more detail than the external one. It is used when the baby doesn’t seem to be doing well. It may also be used when the external monitor is not giving an accurate reading. This can happen if the baby is very active. It can happen when the mother is obese.
* Break your “bag of waters.” Your provider pricks the “bag of waters” with a small tool. The tool enters through the opened cervix. The provider looks at the color of the fluid. Clear is a good sign. Yellow or green could signal a problem.
* Use forceps to help the delivery. Forceps are metal tongs. They are cradled around the baby’s head. They help ease the baby out of the birth canal if the mother can’t push.
* Use vacuum extraction to help the delivery. A suction cup is put on the baby’s head in the birth canal. This helps the baby come out if the mother can’t push. The suction cup is attached to a vacuum pump. Your doctor uses this to pull the baby gently with each contraction. Many doctors prefer this method to forceps. {Note: Forceps and vacuum extraction are not used until the baby’s head can be seen at the vaginal opening.}
* Do an episiotomy. This is a surgical cut. It is made in the skin between the vagina and the anus just before the baby is born. The purpose is to widen the vaginal opening. That helps the baby come out. It also helps keep the skin in the vaginal area from tearing. After the baby is born, the cut is stitched.
How long you stay in the hospital or birthing center will depend on:
* The type of delivery you have and where you give birth. You may go home within 12 to 24 hours in a birthing center. You may be able to stay in a hospital for up to two days. Both of these are with normal vaginal deliveries without problems. C-section stays vary. They usually last 2 to 3 days.
* Your health insurance. Find out what your insurance pays for.
* Your medical needs. You or your baby may need to stay in the hospital longer than usual if you have special medical needs. Sometimes you and your baby get home health care. Your hospital or health insurance may provide this.