You’d never suspect it from the growing number of gluten-free items on supermarket shelves, but only one in about every 133 people has celiac disease. This genetic autoimmune disorder causes the body to react negatively to the intake of gluten, a protein found in wheat, rye, barley, and their byproducts.
It is estimated that more than 80% of the Americans whose systems can’t tolerate gluten are either not diagnosed or misdiagnosed. And the average time a person waits for a correct diagnosis is more than 10 years. A prime reason is that the symptoms of gluten-related problems vary widely-from migraine headaches and diarrhea to joint pain and skin rashes-and are common to numerous other conditions and disorders.
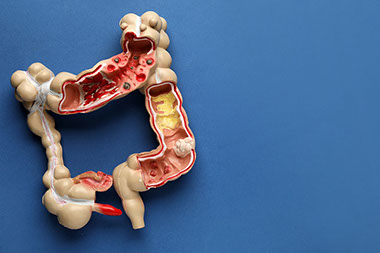
When a person with celiac disease consumes gluten, the protein triggers an immune response that damages part of the small intestine called villi, which interferes with the absorption of nutrients from the food. This can cause malnutrition, trigger other health problems-among them cancer, osteoporosis, and infertility-and open the door to other autoimmune disorders.
“There’s greater awareness of celiac disease, we have better tests, and we know more about who should be screened, but we’re still seeing only the tip of the iceberg,” said Dr. Anca M. Safta, a gastroenterologist at Wake Forest Baptist Medical Center and director of its Gluten & Allergic Digestive Disorders Program.
A simple antibody blood test can screen for celiac disease. And because the disease is inherited, there’s also genetic testing. But while these tests can eliminate the possibility of celiac disease, they can’t confirm its presence. That usually has to be done with an endoscopic biopsy. This procedure examines the small intestine and removes tissue samples for analysis.
If the biopsy results are positive for celiac disease, the only way to repair existing damage to the small intestine and prevent reoccurrence is for the person to adopt a strict gluten-free diet.
That’s also the treatment for people with non-celiac gluten sensitivity. This has symptoms much like those of celiac disease but doesn’t cause the same intestinal damage and can’t be identified through blood or tissue testing.
Steering completely clear of gluten can be tricky. Gluten isn’t just in grain-based products such as bread, cereal, cookies, pastry, pasta, and beer. It also can be found in candy, ice cream, lunch meats, cooking oil, salad dressing, condiments, instant coffee, soup mixes, and a host of other processed foods. Vitamins, toothpaste, and lipstick can also contain gluten.
Gluten-free products are more plentiful than ever, but they’re also costly-nearly 250% more expensive than their conventional counterparts. And because even small amounts of gluten can produce negative effects, cross-contamination-when gluten-free foods come into contact with or are prepared with gluten products-is a threat, especially when eating outside the home.
Is going gluten-free good for everybody? In a word, no.
“It’s not necessarily a healthier diet if you don’t need it,” Dr. Safta said.
Any time you restrict your diet, you have a greater chance of not getting all the nutrients you need. You risk developing a nutrient or vitamin deficiency because gluten-free products aren’t fortified or enriched like most regular bread and cereal products are.
Going gluten-free is not the best way to shed excess pounds. Weight loss is generally due to eating fewer processed foods and more fruits and vegetables, not shunning gluten. And gluten-free foods can contain as many calories as standard products, or even more.