Sexual Health
Sexually transmitted infections (STIs) are ones that pass from one person to another through sexual contact. This can be from vaginal, anal, or oral sex, and from genital-to-genital contact. STIs are also called sexually transmitted diseases (STDs).
Signs & Symptoms
* Primary stage. A large, painless, ulcer-like sore (chancre) appears around the area of sexual contact in 2 to 6 weeks.
* Secondary stage. A month later, a widespread skin rash appears on the palms of the hands, soles of the feet, and sometimes around the mouth and nose. The rash has small, red, scaly bumps that do not itch. Other types of rashes, swollen lymph nodes, fever, and flu-like symptoms may also occur. Small patches of hair may fall out of the scalp, beard, eyelashes, and eyebrows.
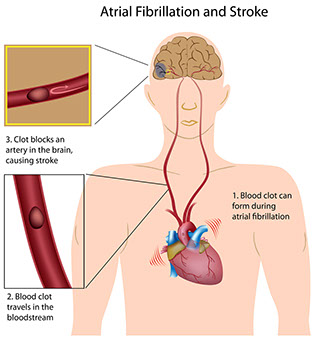
* Latent stage. The infection may go unnoticed for years, but damages the heart, muscles, and other organs and tissues.
Causes
A specific bacterial infection. It can lead to heart failure, blindness, dementia, or death if not treated. {Note: An elderly person with signs of dementia should be evaluated for syphilis. Men and women at an increased risk for syphilis should get screened. Talk to your doctor.}
Treatment
* Antibiotics (usually Penicillin-G given by a shot into the muscle). All persons who have syphilis should be tested for HIV, as advised.
* After treatment, follow-up blood tests are needed in 6 and 12 (and possibly 3) months.
* Once treatment is complete, you’re no longer contagious, but you can get infected again.
Questions to Ask
Self-Care / Prevention
Safer Sex To Help Prevent STIs
* The only sure way to avoid STIs is not having sex. This includes intercourse, oral sex, anal sex, and genital-to-genital contact. Caressing, hugging, dry kissing, and masturbation are no risk or extremely low-risk practices. So is limiting your sexual contact to one person your entire life. This is if your partner does not have an STI and has sex only with you.
* Latex and polyurethane condoms can help reduce the risk of spreading HIV and other STIs (i.e., chlamydia, gonorrhea, and trichomoniasis). To do this, they must be used the right way for every sex act. They do not get rid of the risk entirely. Barriers made of natural membranes, such as from lamb, do not give good protection against STIs.
* Females and males should use latex or polyurethane condoms every time they have genital-to-genital contact and/or oral sex. Use polyurethane condoms if either partner is allergic to latex. You don’t need condoms to prevent STIs if you have sex only with one partner and neither of you has an STI.
* For oral-vaginal sex and oral-anal sex, use latex dams (“doilies”). These are latex squares.
* Latex condoms with spermicides, such as nonoxynol-9 (N-9) are no better than other lubricated condoms for preventing HIV/STIs. Spermicides with N-9 do not prevent chlamydia, cervical gonorrhea, or HIV. on’t use spermicides alone to prevent HIV/STIs. Using spermicides with N-9 often has been linked with genital lesions which may increase the risk of spreading HIV. Also, N-9 may increase the risk of spreading HIV during anal intercourse.
* Use water-based lubricants, such as K-Y Brand Jelly. Don’t use oil-based or “petroleum” ones, such as Vaseline. They can damage latex barriers.
* To lower your risk for HPV, use latex or polyurethane condoms. These work best at covering areas of the body that HPV is most likely to affect. A diaphragm does not prevent the spread of HPV.
* Don’t have sex while under the influence of drugs or alcohol. You are less likely to use “safer sex” measures.
* Limit sexual partners. Sexual contact with many persons increases the risk for STIs, especially if no protection is used.
* Discuss a new partner’s sexual history with him or her before you start having sex. Know that persons are not always honest about their sexual past.
* Avoid sexual contact with persons whose health status and health practices are not known.
* Follow your doctor’s advice to check for STIs.
Resources
American Social Health Association (ASHA)
CDC National STD Hotline
800.CDC.INFO (232.4636)