Some foot problems are due to years of wear and tear on your feet. Others can be due to shoes that do not fit well or trimming your toenails too close to your skin. Circulation problems and diseases, such as diabetes, can lead to foot problems, too.
{Note: If you have diabetes or circulation problems, contact your doctor for any foot problems.}
To Help Prevent Foot Problems
* Maintain a healthy weight to avoid excess strain on your feet.
* Wear shoes that fit well. Don’t wear shoes with pointed toes or ones that fit too tightly.
* Wash and dry your feet daily.
* Keep your feet moisturized.
* Inspect your feet daily for signs of problems.
* Rest your feet by elevating them.
* Persons with diabetes and/or circulation problems need to take special care of their feet. Good foot care can prevent some foot infections. It may be necessary for a health care professional to cut the toenails.
R.I.C.E.
* Rest the injured area for 24 to 48 hours.
* Ice the area as soon as possible. Keep doing this for 10 minutes every 2 hours for the first 48 hours. Use an ice pack, ice in a heavy plastic bag with a little water, a bag of frozen vegetables, etc. Put a thin towel between the ice pack and the skin.
* Compress the area. Wrap with an elastic bandage. Do not cut off circulation. Remove the bandage every 3 to 4 hours, for 15 to 20 minutes each time.
* Elevate the area above heart level, if possible. Place it on a pillow, folded blanket, stack of newspapers, etc.
Athlete’s Foot
Signs & Symptoms
Moist, soft, red, or gray-white scales on the feet, especially between the toes. Cracked, peeling, dead skin area. Itching. Sometimes small blisters on the feet.
What to Do
SeeAthlete’s Foot.
Blisters
Signs & Symptoms
Red, sometimes fluid-filled sores caused by shoes that rub the foot.
Self-Care / Prevention
* Don’t break a blister. If it breaks on its own, apply an antibacterial spray or ointment and cover with a bandage or sterile dressing.
* Don’t cut away or pull off the broken blister’s loose skin. This protects the new skin below it.
Broken Bone(s) in the foot (not just a toe).
Signs & Symptoms
Pain from a fall or injury to your foot (not just a toe) with any of these problems:
* Severe bleeding.
* Your foot is misshaped.
* You can’t move your foot.
* Your foot looks blue or pale and is cold and numb.
* Your foot is so painful and/or swollen that you can’t put any weight on it.
What to Do
Get medical care fast!
Broken or Sprained Toe
Signs & Symptoms
Pain in only one toe after an injury to the toe.
Buerger’s Disease
Signs & Symptoms
Open sores (ulcers) on the toes. Pain on the instep and cold, pale skin color which improves with rest.
What to Do
See doctor.
Bunion
Signs & Symptoms
The big toe points inward or outward. A bony bulge at side of the big toe. Thickened skin. Possible fluid build-up near the big toe. Stiffness or pain.
Self-Care / Prevention
* Don’t wear high heels or shoes with narrow toes.
* Wear sandals.
* Use moleskin or padding to separate overlapped toes.
* Try arch supports to reduce pressure.
* Use ring-shaped pads over a bunion.
* Cut out an old pair of shoes to wear in the house.
* Soak your feet in warm water.
* If needed, take an over-the-counter pain reliever as directed.
Callus
Signs & Symptoms
Thickened skin on the ball or heel of the foot. Usually no pain.
Cellulitis
Signs & Symptoms
The bottom of the foot is red and swollen and feels warm and tender.
What to Do
SeeCellulitis.
Corn
Signs & Symptoms
Thickened skin on tops of and between toes where rubbing is constant. Feels hard to the touch and looks round. Small, clear spot (hen’s eye) may appear in the center.
Cut or Puncture Wound
Signs & Symptoms
Cut or puncture from a dirty or contaminated object, such as a rusty nail or other object in the soil.
Foot Cramp
Signs & Symptoms
Charley horse or muscle spasm in the foot. Often, this occurs at bedtime.
Self-Care / Prevention
* Stretch the foot muscles.
* Pull the foot back into a flexed position.
* Push the foot into the floor.
Frostbite (if signs occurs after cold exposure).
Signs & Symptoms
Toes turn white then red in response to cold. Tingling. Numbness.
What to Do
Contact doctor for an appointment right away.
Gangrene
Signs & Symptoms
These problems appear in a matter of hours to a few days:
* The skin of your foot or toe is gray to black in color.
* You cannot feel sensation in your foot.
What to Do
Get medical care fast!
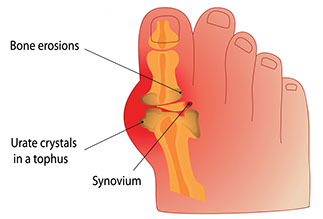
Gout
Signs & Symptoms
Severe pain in foot joint, often the big toe. The pain is not due to an injury. The joint hurts a lot when anything touches it. The area is red, swollen, and tender.
What to Do
See doctor.
Hammertoe
Signs & Symptoms
Curled or claw-like position in a toe (usually the 2nd toe). A corn forms on the top of the toe. Pain.
Self-Care / Prevention
* Wear wide, roomy shoes.
* Massage the toes or get a foot rub.
* Change shoes during the day. Try athletic shoes.
* Use small pads over the center of the toe to lessen pressure.
Heel Spur
Signs & Symptoms
Tenderness and pain under the heel bone.
What to Do
See doctor.
Self-Care / Prevention
* Use a cushion or heel cup under the heel.
* Do not jog or run. Avoid prolonged standing.
* Lose weight, if overweight.
* Roll a tennis ball under ball of the foot.
* Put ice on the heel for 10 minutes. Remove it for 10 minutes. Repeat many times.
* If needed, take an over-the-counter pain reliever as directed.
Infection
Signs & Symptoms
A foot wound with: Fever; redness, tenderness, or warmth; swelling; pain; and/or pus.
What to Do
See doctor.
Self-Care / Prevention for Minor Infections
* Soak the foot in warm, soapy water for 20 minutes, 4 to 6 times a day. Pat the infected area dry. Use extra care if you have peripheral vascular disease. Make sure the water is not hot.
* Apply an over-the-counter antibiotic ointment, such as Neosporin. Cover with a sterile cloth or bandage.
Ingrown Toenail
Signs & Symptoms
Discomfort, pain, tenderness, and/or redness under the corner of a toenail and nearby skin.
Morton’s Neuroma
This is thickening of nerve tissue, usually between the third and fourth toes.
Signs & Symptoms
Sharp and burning pain on the ball of the foot.
Self-Care / Prevention
* Wear wide shoes with soft insoles.
* Put pads or arch supports in your shoes. These help take pressure off the area.
* Take an over-the-counter medicine for pain as directed.
* See your doctor if the above measures don’t bring relief.
Peripheral Vascular Disease
Signs & Symptoms
Sudden onset of pain in your feet and legs. The skin on your feet rapidly changes color: white, red, blue, grayish, or black.
What to Do
Get medical care fast!
Planter Fasciitis
This is a problem with ligaments and tissues in the foot arch.
Signs & Symptoms
Pain between the heel and the ball of the foot. Often this is due to walking, running, or putting weight on the foot.
Self-Care / Prevention
* Rest the foot as much as you can.
* Use R.I.C.E.
* Take an over-the-counter medicine for pain and swelling as directed.
* Wear shoes with a solid arch support.
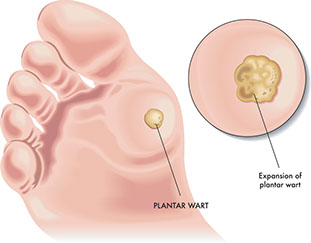
Planter Wart
Signs & Symptoms
Painful growth on the ball or heel of the foot. Black pinholes or spots in the center.
Self-Care / Prevention
* Try salicylic acid plasters or other over-the- counter products, such as Wart-Off. Follow package directions.
* Use cushions in shoes.
* Wash your hands after touching warts to avoid re-infection.
* Wear sandals in the shower or public areas, such as pools.
* Do not pick at plantar warts.
Rheumatoid Arthritis
Signs & Symptoms
Joint pain and morning stiffness in joints that lasts more than 1 hour. Fatigue.
What to Do
See doctor.
Toenail Fungus
Signs & Symptoms
White, brown, or yellow toenail. The nail can thicken, then get soft and weak. It may tear away from the nail bed or look deformed.
What to Do
See doctor.